Liver Transplantation:警惕!脂肪肝日渐成为常见病
2016-04-13 佚名 生物谷
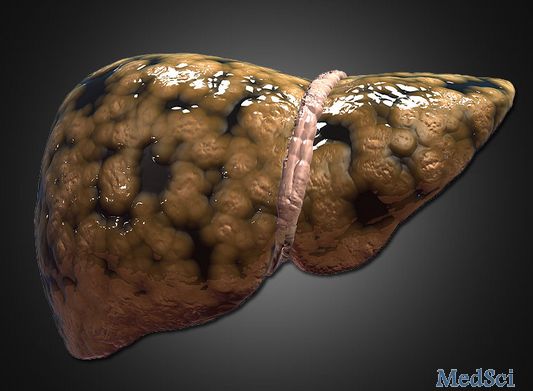
图片摘自:www.medscape.com 近日,刊登在Liver Transplantation杂志上的一项研究报告中,来自国外的研究人员分析了肝脏移植患者机体脂肪肝疾病的流行特征及风险因子,相关研究为后期开发新型策略来保护器官移植患者的健康或将提供一定的研究线索。 脂肪肝(Steatosis),即肝脏被脂肪所浸润,通常发生于肝脏移植患者中,但目前研究者并不清楚脂肪肝在肝脏移植患者中的

图片摘自:www.medscape.com
近日,刊登在Liver Transplantation杂志上的一项研究报告中,来自国外的研究人员分析了肝脏移植患者机体脂肪肝疾病的流行特征及风险因子,相关研究为后期开发新型策略来保护器官移植患者的健康或将提供一定的研究线索。
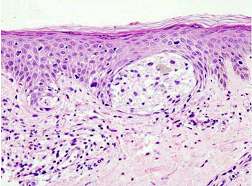
脂肪肝(Steatosis),即肝脏被脂肪所浸润,通常发生于肝脏移植患者中,但目前研究者并不清楚脂肪肝在肝脏移植患者中的实际流行特征,同时也并不清楚相关的风险因子以及如何改善肝脏移植患者的生存率。为此本文研究中研究人员对来自548名肝脏移植患者机体的肝脏活检及生存率数据进行了一项回顾性分析和研究。
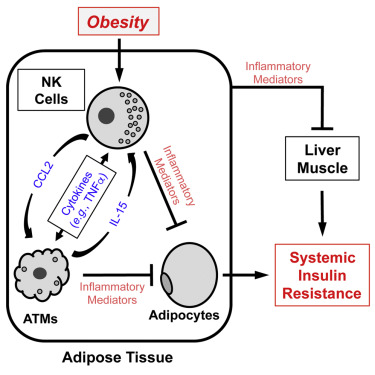
研究者上述研究对象中发现了309名脂肪肝患者(56.4%),其中包括93名(17.0%)明显的脂肪肝患者,研究者指出,进行肝脏移植后患者机体脂肪肝的流行率从1年时的30.3%增加到了10年后的47.6%;当研究者对患者在移植前的特性进行分析后他们发现,因饮酒而引发的较高体重指数和肝硬化往往和患者患脂肪肝之间存在明显关联,通过分析患者移植肝脏后的表现,研究者发现,较高的体重指数、高血脂、饮酒及2型糖尿病和患者患脂肪肝存在一定关联;这就表明,数年内肝脏移植后患者患脂肪肝和患者较差的生存率之间并没有关联,但严重脂肪肝患者的长期生存率或会趋于更加严重。
最后研究者Hejlova说道,我们的研究首次对大量欧洲肝脏移植患者进行研究,描述了这些患者脂肪肝的发生、进展及其它特性;脂肪肝的发生表明这些患者长期的存活率或许会受到影响,对于这些患者而言肥胖可以避免,而且患者也应该被鼓励增加体育锻炼来改善疾病的进展;研究者提示,对糖尿病和高血脂症进行筛查和治疗,以及限制饮酒对于有效改善肝脏移植患者脂肪肝疾病的进展以及患者的生存率或提供一定帮助。
原始出处:
Irena Hejlova,et al.Prevalence and risk factors of steatosis after liver transplantation and patient outcomes.Liver Transplantation.5 April 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TRA#
30
#Transplantation#
31
#常见病#
37
#Transplant#
26
#plant#
39
高大上的文章
172
值得学习
115
现代饮食作息的改变。
114