纵隔淋巴结肿大(转移、结节病)丨影像表现
2022-10-23 熊猫放射 熊猫放射
多系统慢性炎症性疾病,以非干酪性肉芽肿为特征最佳诊断线索:双肺门对称性及右侧气管旁肿大淋巴结CT:相应区域淋巴结肿大,可见钙化。
结节病丨影像表现
转移性疾病,淋巴结肿大
Metastatic Disease, Lymphadenopathy
影像表现:
最佳诊断线索:CT上胸部淋巴结≥10mm,PET/CT上FDG摄取增高
CT:淋巴结增大,短径≥10mm;低密度,有强化,有/无钙化;胸内/外恶性肿瘤的特异性淋巴引流通路
PET/CT:淋巴结内FDG摄取增高,容易发现肺癌淋巴结转移、食管癌局部淋巴结转移;假阳性:肉芽肿性疾病、感染/炎症
鉴别诊断
-
淋巴瘤
-
结节病
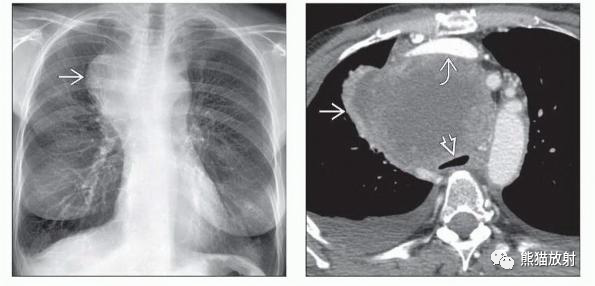
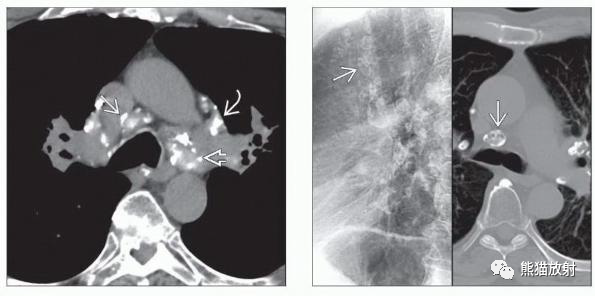
(左) 转移性黑色素瘤患者,PA胸片显示右上纵隔巨大软组织肿块。
(右) 同一患者的轴位CECT显示纵隔气管前区巨大软组织肿块,密度不均,气管明显受压,纵隔血管移位。这类肿块为广泛融合的转移性纵隔增大淋巴结。
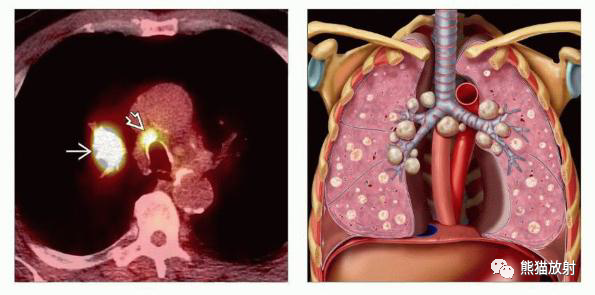
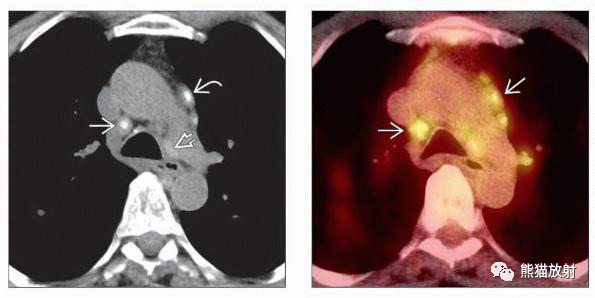
(左) 原发性肺癌并纵隔淋巴结转移,PET/CT显示右肺结节和气管右旁淋巴结FDG代谢增高,分别对应原发性和转移性肺癌。
(右) 图示晚期恶性肿瘤的典型特征,表现为双肺多发转移,双侧恶性胸腔积液,肺门和纵隔淋巴结转移。

(左) 肺癌患者,左肺较大软组织肿块,密度较低,纵隔内左、右气管旁和主肺动脉窗区可见融合性的软组织密度灶。双侧胸腔少量积液。
(右) 同一患者,双侧锁骨上淋巴结肿大,为N3型,IIIB期,排除手术切除的可能。
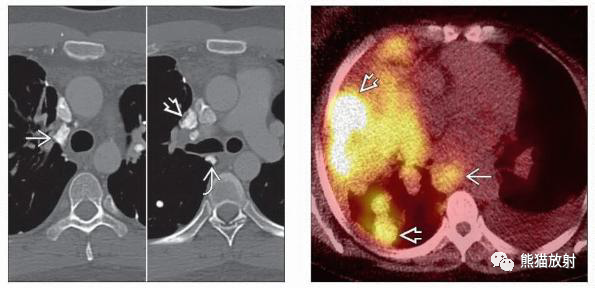
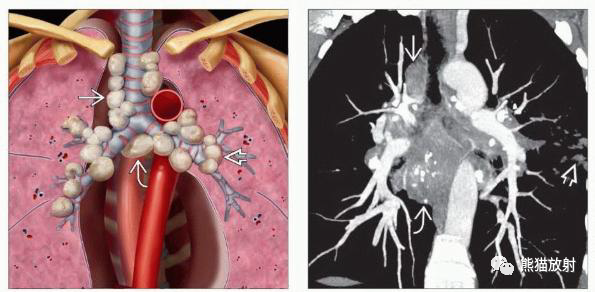
(左) 骨肉瘤患者,气管右旁、右肺门和隆突下淋巴结增大并钙化。结肠和卵巢的粘液腺癌、甲状腺癌和骨肉瘤可导致钙化性淋巴结转移。
(右) 转移性乳腺癌患者,PET/CT显示隆突下淋巴结FDG摄取,胸膜转移灶FDG摄取增高。

(左) 转移性肝细胞癌患者,CECT显示纵隔淋巴结多发转移,密度不均。胸外恶性肿瘤的淋巴结转移远不如胸内恶性肿瘤的淋巴结转移常见。
(右) 原发性左肺上叶肺癌,并主肺动脉窗淋巴结转移。
结节病,淋巴结肿大
Sarcoidosis, Lymphadenopathy
概述:
-
多系统慢性炎症性疾病,以非干酪性肉芽肿为特征
最佳诊断线索:双肺门对称性及右侧气管旁肿大淋巴结
CT:相应区域淋巴结肿大,可见钙化
鉴别诊断:
-
淋巴瘤
-
转移性疾病
-
感染
-
尘肺
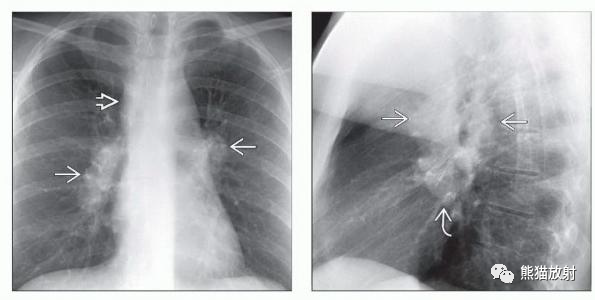
(左) 结节病患者,PA胸片显示双肺门增大和气管右旁增厚,代表淋巴结增大。
(对) 同一患者,侧位片显示双肺门和隆突下淋巴结增大。约95%的结节病患者发生胸内淋巴结增大。大约90%的病例发生肺门/纵隔淋巴结增大和肺受累。
(左) 双肺门、气管右旁和隆突下淋巴结增大。
(对) 2期结节病患者,双肺门、气管右旁和隆突下多发肿大淋巴结,可见点状钙化。结节病的特征是增大淋巴结的对称性分布,可见双肺簇状分布的肺结节。
(左) 长期结节病患者,纵隔多发增大淋巴结并钙化。
(右) 结节病,多发纵隔及肺门增大淋巴结,外周壳状钙化在胸部CT上显示清晰。淋巴结钙化的发生率随疾病持续时间增加。

(左) 结节病,X线片显示双肺门淋巴结肿大。
(右) 结节病,CECT显示胸内广泛淋巴结增大,影响气管右旁、血管前、前纵隔和双侧内乳淋巴结。
(左) 轴位NECT显示左、右气管旁和血管前淋巴结无明显增大,内见钙化。
(右) 同一患者,PET/CT显示这些淋巴结FDG摄取增加。PET/CT不能区分结节病相关的淋巴结肿大与继发于淋巴瘤、转移性疾病、感染或尘肺的淋巴结肿大。然而,PET/CT可以用来监测治疗反应。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







留存学习
43
转发学习
36
感谢分享
37
如果能注明分区可能会更好一点
37
学习了,谢谢分享
39
虽然还是有点懵(自身原因),但还是获得了许多知识。
25
认真学习了
31