JACC:隐匿性心梗患者应警惕心衰
2018-01-08 许菁 中国循环杂志
据社区人群动脉粥样硬化风险(ARIC)队列研究最新结果,心电图意外发现隐匿性心肌梗死不可掉以轻心,因其发生心衰风险高。
以前在ARIC研究曾发现隐匿性心肌梗死与全因死亡率的增加有关,目前的研究又发现其也与心衰有关,这提示隐匿性心肌梗死与有症状的心肌梗死一样严重。
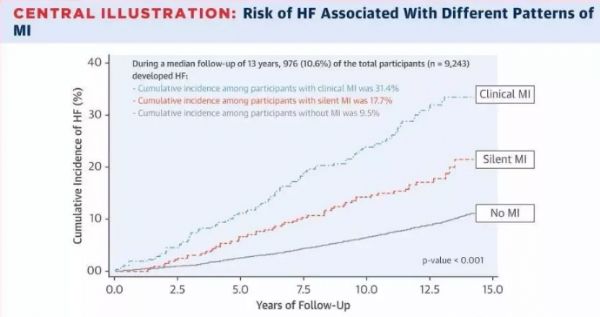
这项新的研究纳入9243名基线无心血管疾病的受试者。该队列中, 10.6%的受试者在中位随访13 年时首次心衰住院。有症状心肌梗死患者的心衰累积发生率为31.4%,心电图识别的新发的隐匿性心肌梗死患者的心衰累积发生率为17.7%。无心肌梗死者的心衰的累积发生率为9.5%。
与那些无心肌梗死的受试者相比,隐匿性心肌梗死患者发生心衰的风险增加35%。
研究者表示,虽然目前的研究还不能直接证明隐匿性心肌梗死是的心力衰竭的原因,但心脏电活动异常意味着心肌有损伤,这与心功能有直接的关系。因此隐匿性心肌梗死应看作冠心病的一个危险因素。
原始出处:
Qureshi WT, et al. Silent myocardial infarctionand long-term risk of heart failure. The ARIC Study. J Am Coll Cardiol, 2018,71: 1-8.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JACC#
0
#心梗患者#
31
#隐匿性#
29
#ACC#
21
#隐匿#
25