Clin Cancer Res:地西他滨联合PARP抑制剂他唑帕尼治疗难治性/复发性急性髓性白血病
2022-02-24 xiaozeng MedSci原创
地西他滨/他唑帕尼联合使用在复发性/难治性 AML 患者中的耐受性良好,而且有初步的抗肿瘤活性
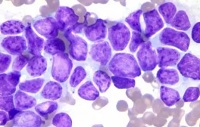
不适合强化化疗或对强化化疗有耐药性的急性髓性白血病 (AML) 患者通常使用 DNA 甲基转移酶抑制剂 (DNMTi) 治疗。新的药物联合方案或可增加疗效。除了使 CpG 岛基因启动子区域去甲基化,DNMTi 还可增强 PARP1 的招募和与染色质的紧密结合,从而阻断 PARP 介导的 DNA 修复,进而下调同源重组 (HR) DNA 修复,最终增加肿瘤细胞对 PARP 抑制剂(PARPi)的敏感性。
Maria 等研究人员既往已在体内外证实了 DNMTi 和 PARPi 联合使用在 AML 中的效果。在本研究中,Maria 等研究人员在复发性或难治性 AML 患者中探索了 DNMTi 地西他滨和 PARPi 他唑帕尼联合使用时推荐的2期剂量,以及初始活性和安全性。
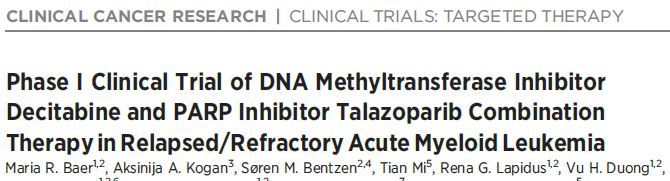
剂量递增方案
招募了年满 18 岁的明确诊断的经既往治疗后进展或难治性的、且对强化化疗不耐受或不敏感的 AML 患者。28天为一疗程,每疗程连续5-10天予以地西他滨,每疗程的第1天予以他唑帕尼。并在第1天(预处理)、第5天和第8天进行药效学分析。
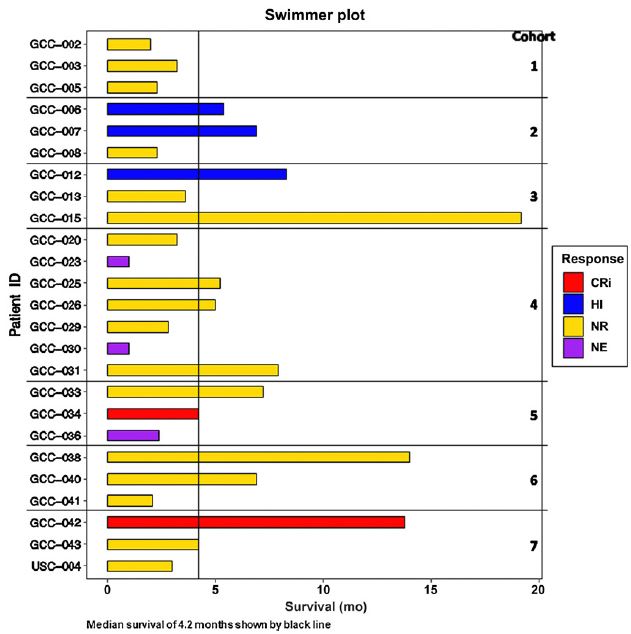
共招募了 25 位患者,其中 22 位既往接受过 DNMTi 治疗。受试患者被分成了 7 个队列,采用剂量递增的3+3设计。推荐的 2 期两联合剂量方案是:连续予以地西他滨(20 mg/m2)5-10天+每疗程的第 1 天予以他唑帕尼(1 mg),28天为一疗程。
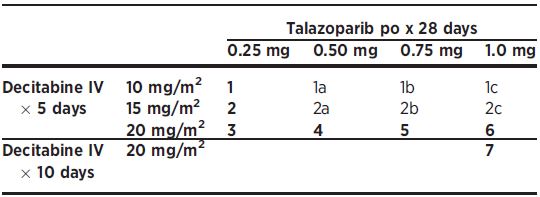
非血液学副作用
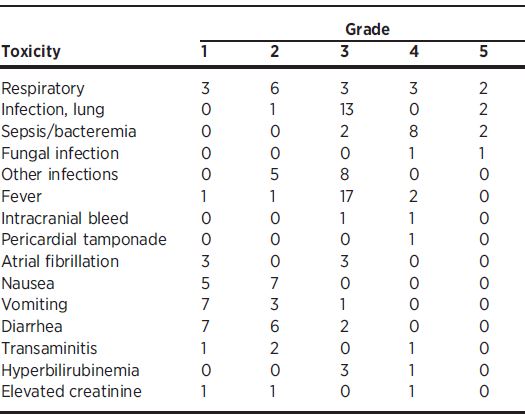
3-5级的副反应有发热(19例)和肺部感染(15例)。两位患者(8%)获得了细胞计数不完全恢复的完全缓解,另有三位患者的血液学有所改善。
所有患者的治疗反应
药效学分析证实了预期的 DNA 去甲基化、染色质 PARP 捕获增加、γH2AX 位点增多和缓解者的 HR 活性降低。与20 mg/m2地西他滨联合使用时,γH2AX 位点随着他唑帕尼剂量的增加而增多。
综上,地西他滨/他唑帕尼联合使用在复发性/难治性 AML 患者中的耐受性良好,而且有初步的抗肿瘤活性,值得进一步研究。
原始出处:
Maria R. Baer, et al. Phase I Clinical Trial of DNA Methyltransferase Inhibitor Decitabine and PARP Inhibitor Talazoparib Combination Therapy in Relapsed/Refractory Acute Myeloid Leukemia. Clin Cancer Res (2022). https://doi.org/10.1158/1078-0432.CCR-21-3729
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#复发性#
53
#抑制剂#
35
#地西他滨#
76
学习了
65
学习学习
74
#髓性#
51
#难治性#
39
#PARP#
33