Cell Host & Microbe:新年才想起健康饮食 肠道菌群说:迟咯
2017-01-03 pippi 生物360
这个新年当你试图改善你的饮食习惯,你的肠道微生物群可能变化不大。发表在 Cell Host & Microbe 一项新研究中,研究人员探索了:小鼠从无限制的美国饮食转换到健康的、卡路里限制的、偏素食的饮食,它们对这样的改变并未及时响应。研究者发现某些人类肠道细菌需要新年丢失,变更的饮食计划才得以成功。 Griffin等人的发现:对饮食干预的微生物群响应的幅度随个体而变化,
这个新年当你试图改善你的饮食习惯,你的肠道微生物群可能变化不大。发表在 Cell Host & Microbe 一项新研究中,研究人员探索了:小鼠从无限制的美国饮食转换到健康的、卡路里限制的、偏素食的饮食,它们对这样的改变并未及时响应。研究者发现某些人类肠道细菌需要新年丢失,变更的饮食计划才得以成功。

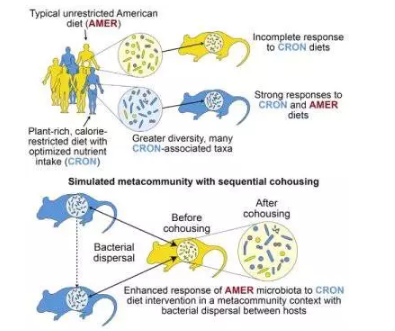
Griffin等人的发现:对饮食干预的微生物群响应的幅度随个体而变化,宿主之间饮食反应性细菌分类物的分散增强了随后对饮食干预的反应。Credit: Griffin et al. / Cell Host & Microbe
华盛顿大学圣路易斯市华盛顿大学(WUSTL)基因组科学与系统生物学中心主任 Jeffrey Gordon(本论文的资深作者)说:“如果我们要开饮食处方来改善某人的健康,我们就必须了解什么微生物能够帮助控制这些有益的效果。我们已经找到了一种方法来挖掘不同人类的肠道微生物群落,以识别有助于促进特定饮食效应的生物体。”
为了研究人类饮食习惯如何影响人类肠道微生物群,以及从如常的饮食生活方式变成新规定的饮食方式微生物群是怎样做出反应的。Gordon 和他的合作者首先采集了遵循卡路里限制、植物丰富的饮食者的粪便样品,和来自遵循典型的、无限制的美国饮食者的粪便样品。研究人员发现,遵循卡路里限制、植物丰富的饮食方式的人具有更多样化的微生物群。
然后研究者给无菌小鼠接种不同的人类供体肠道微生物群落,并给小鼠饲喂供体的常规饮食或其他饮食类型。虽然两组小鼠对新饮食习惯做出了反应,但具有典型美国饮食调节的微生物群的小鼠对于富含植物的饮食具有较弱的反应。
为了鉴定可以增强美国饮食调节的微生物群的反应的微生物,研究人员在小鼠之间建立了一系列的阶段共饲养。含有美国饮食调节的生物群落的小鼠,顺序地与来自不同人的植物饮食微生物群落的小鼠共同饲养。研究结果表明,来自植物饮食调节的微生物进入美国饮食调节的微生物群,显着改善其对植物饮食的反应。
“我们的肠道微生物群落不是孤立的岛屿,而是作为群岛的一部分,肠道微生物可以从岛屿移动到岛屿,我们称这个群岛是一个集合群落metacommunity,”第一作者,WUSTL 的讲师 Nicholas Griffin 说,“许多迁移到美国饮食调节的微生物群落的肠道细菌,最初在很多非限制性饮食的肠道微生物中不存在。”
尽管科学家们乐观地认为,他们的研究将有助于指导新策略的发展,以提高健康饮食的处方的效率,他们强调,需要更多的研究来确定决定人与人之间微生物交流的因素。
“我们对于营养价值和饮食的影响如何影响消费者的微生物群落越来越欣赏,”Gordon 说,“我们希望本研究中描述的鉴定微生物的方法,可能有一天被用作下一代益生菌。我们的微生物提供了另一种方式来强调,在一个大的群落中,我们人类如何彼此之间相互联系的。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
34
#Micro#
28
#CRO#
34
迟到总比不到好
62
#Cell#
28
#肠道菌#
34