European Radiology:CT灌注预测的梗死核心与急性卒中临床结果之间的关系
2022-04-19 shaosai MedSci原创
研究表明,CTP衍生的pIC可能会大幅高估缺血性改变,在早期完全再灌注的情况下尤为显著。
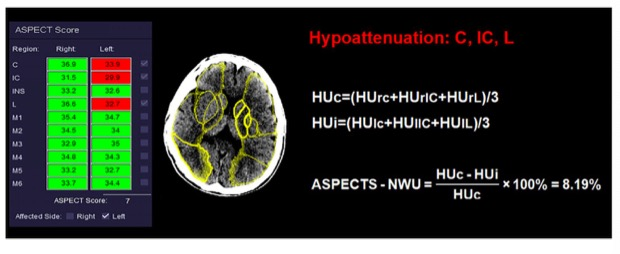
 评估梗死区的非活性组织或梗死核心是评估急性卒中患者病情最重要的基线影像学标志之一。梗死核心可以通过几种不同的技术来估计,如平扫CT中的ASPECTS、CT灌注(CTP)中脑血容量或脑血流(CBF)以及磁共振成像中扩散加权成像。
评估梗死区的非活性组织或梗死核心是评估急性卒中患者病情最重要的基线影像学标志之一。梗死核心可以通过几种不同的技术来估计,如平扫CT中的ASPECTS、CT灌注(CTP)中脑血容量或脑血流(CBF)以及磁共振成像中扩散加权成像。
由于CTP的临床可用性较高,该技术被广泛用于急性卒中以获得预测的梗死核心(pIC)体积。尽管pIC与临床结果指标之间存在整体关联,但一些治疗前和治疗相关的变量也可以改变这些关系,包括年龄、基线国家卫生研究院卒中量表(NIHSS)、ASPECTS、CTP获取时间、再灌注程度、旁路或高血糖状态。具体来说,CTP衍生的pIC可能会大幅高估缺血性改变,在早期完全再灌注的情况下尤为显著。因此,更好地界定这些变量之间的相互作用,对保证在早期卒中中的更好的结果预测意义重大。
近日,发表在European Radiology杂志的一项研究在假设pIC的预后准确性可被一些基线和治疗相关的变量所改变的情况下,在一个患有大血管前循环闭塞的急性缺血性卒中患者队列中,对所有患者在卒中发生后8小时内进行CTP成像,以明确pIC和临床预后之间最相关的改变因素。
本研究纳入了828名患有急性颈动脉近段闭塞患者,这些患者在卒中发生后8小时内接受了全脑CTP成像。在CTP地图上计算pIC(脑血流<30%),不良的临床结果被定义为90天改良的Rankin评分>2。通过对派生队列(n = 654)的一阶和高级互动分析,评估pIC和临床结果之间的潜在中介因素以获得预测模型。在一个独立的队列(n = 174)中进一步验证了衍生的模型。
pIC的体积与不良的临床结果不良显著相关(OR = 2.19,95% CI = 1.73 - 2.78,P < 0.001)。这种关联的强度取决于基线国家卫生研究院卒中量表、葡萄糖水平、使用血栓切除术以及年龄与血栓切除术的相互作用。在推导队列和验证队列中,结合这些变量的模型对预测临床结果显示出良好的分辨力(受试者工作特性曲线下面积分别为0.780(95%CI=0.746-0.815)和0.782(95%CI=0.715-0.850))。

图 应用该模型的代表性示例(A),不同程度的暴露于所确定标志物的汇总表(B)。CBF:脑血流;DT:延迟时间;mRS:改良的Rankin量表评分;MT:机械血栓切除术;NIHSS:美国国立卫生研究院卒中量表;pIC:预测梗死核心
本研究提示,CTP衍生的pIC在预测急性缺血性卒中患者部分亚组临床结果方面的准确性有限,这些亚组是在卒中发生后8小时内成像、并由特定的基线或治疗变量定义。同时,增加某些简单的基线临床变量会提高由pIC估计得出的结果预测的准确性。因此,本研究结果表明,在评估pIC的预后价值时,必须同时考虑这些变量对结果影响。
原文出处:
Carlos Laredo,Aleix Solanes,Arturo Renú,et al.Clinical and therapeutic variables may influence the association between infarct core predicted by CT perfusion and clinical outcome in acute stroke.DOI:10.1007/s00330-022-08590-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#临床结果#
60
#PE#
46
#学习#学习
51
#学习#学习
52
#急性卒中#
47