J Am Coll Cardiol:我国仅有很少部分人拥有健康心脏?!
2015-03-10 佚名 生物谷
将近四分之三的中国成年人的心血管处于亚健康。这是伴随着不良的饮食习惯和肥胖人群的增多,加上持续走高的吸烟人群。这个结果是根据上海交通大学一群科研人员发表在Journal of the American College of Cardiology上的最新成果得到的。 2010年中国非传染性疾病监测协会从具有全国代表性的超过96000个男性和女性中采集心血管健康数据。据调查结果得出估计,只有0.2

将近四分之三的中国成年人的心血管处于亚健康。这是伴随着不良的饮食习惯和肥胖人群的增多,加上持续走高的吸烟人群。这个结果是根据上海交通大学一群科研人员发表在Journal of the American College of Cardiology上的最新成果得到的。
2010年中国非传染性疾病监测协会从具有全国代表性的超过96000个男性和女性中采集心血管健康数据。据调查结果得出估计,只有0.2%的中国男性和女性享受“理想”的心血管健康(理想的健康状态是根据美国心脏协会提出的7大健康的行为/健康因素而定义)。
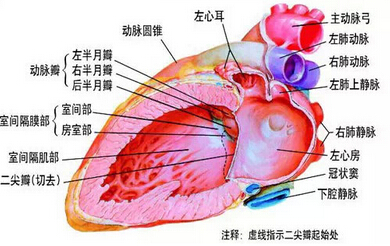
考虑到目前,心脑血管疾病已经称为中国主要死因。交大的研究人员开始评估中国成年人当前心血管健康的状态。研究者将无心血管疾病史的参与者按健康行为习惯及身体条件按理想水平,中间水平,和较差水平分类。这其中包括:四个健康行为习惯——吸烟状况;体重指数(BMI);锻炼活动;饮食;三个健康身体因素——未处理/治疗过的总胆固醇水平;未经治疗过的血压水平;和未经服药的空腹血糖水平。
研究人员发现,接受调查的更多的中国女性比男性有理想的心血管健康,百分比分别为0.4%和0.1%。拥有四个理想行为习惯的女性的百分比男性也略高:分别是1%对0.4%。同样,22.3%的女性,相比于5%的男性拥有四个理想的健康因素。在这项研究中,体重指数被考虑为行为习惯,而吸烟状况被考虑既是行为也是健康的因素。
总之,43.4%的男性被报告为从不吸烟或已戒烟超过12个月,相比女性97.3%的比例。女人与男性相比,也更可能有理想的血压和血糖水平。七个指标中,坚持健康的饮食习惯是所有心血管健康指标中最不常见的,拥有者仅占1.6%,在男性和女性之间都相似。
研究人员还之处中国糖尿病的患病率比过去十年增加了一倍多,而吸烟率,主要是男性,仍然很高。
研究人员表示:“中国是世界上人口最多的国家。改变了中国人群的患病率会显著影响全球疾病负担。获得国家心血管健康数据,以及随着时间的推移更新追踪其变化,对于中国是至关重要的。”
原始出处:
Status of Cardiovascular Health in Chinese Adults.JACC March,2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cardiol#
38
#Coll#
34
应该好好改变
103
不良生活习惯的中国人
117
明白了
115