Thorac Cancer:术后放疗可提高新辅助化疗+术后病理为ypN2的非小细胞肺癌患者的生存:来自SEER数据库倾向评分匹配分析
2021-12-18 yd2015 MedSci原创
研究表明,对于新辅助化疗术后的ypN2 NSCLC患者,术后放疗(PORT)可改善患者的OS和CSS。
对于新辅助化疗后进行手术后病理为ypN2的非小细胞肺癌(NSCLC)患者术后放疗(PORT)的作用尚不清楚。北京大学肿瘤医院的团队基于SEER数据库,评估PORT对ypN2 NSCLC患者术后生存的影响。相关结果发表在Thoracic Cancer杂志上。

研究从SEER数据库筛选2004年至2015年新辅助化疗术后的ypN2 NSCLC患者。使用倾向评分匹配(PSM)来平衡术后放疗(PORT)组和非术后放疗(PORT)的基线特征。采用Kaplan Meier法和Cox比例风险模型估计总生存期(OS)和癌症特异性生存期(CSS)。
纳入257例患者,中位年龄63岁(范围35-89岁),中位阳性淋巴结数为3个(范围0 - 38)。大约一半的患者(53.7%)是IIIA期。132例(51.4%)患者接受PORT治疗。PORT组晚期患者或区域淋巴结阳性更多。经PSM匹配后,两组患者各性状平衡良好,每组有115例。
中位随访时间为82个月(范围41-51个月)。PSM前,PORT组中位OS为36个月(95% CI: 30 58个月),非PORT组中位OS为25个月(95% CI: 19-32个月)。5年OS率分别为38.2% (95% CI: 30.0% -48.5%)和21.2% (95% CI: 14.9-30.2%) (p = 0.003)。PORT组的中位CSS为38个月(95% CI: 32-69个月),PORT组为26个月(95% CI: 21-34个月)。5年CSS发生率分别为41.3% (95% CI: 32.9%- 52.0%)和22.45% (95% CI: 15.8%-31.9%) (p = 0.001)。PSM后,PORT仍然显著提高生存率。两组患者中位OS分别为36个月(95% CI: 30-69个月)和26个月(95% CI: 21-32个月),5年OS率分别为40.5% (95% CI: 31.9%-51.4%)和21.0% (95% CI 14.5%-30.5%) (p = 0.002)。中位CSS为38个月(95% CI: 32-77个月)和27个月(95% CI: 21-36个月),5年CSS发生率分别为43.7% (95% CI: 34.8%-54.8%)和22.1% (95% CI: 15.3%-31.9%) (p<0.001)。

在多变量分析中,PORT被确认为OS (HR = 0.59, p = 0.001)、CSS (HR = 0.56, p = 0.001)的独立预后因素。同样还有年龄(OS: HR = 1.60, p = 0.01;CSS: HR = 1.58, p = 0.02)和T分期(OS: HR = 1.54, p = 0.01;CSS: HR = 1.56, p = 0.01)。
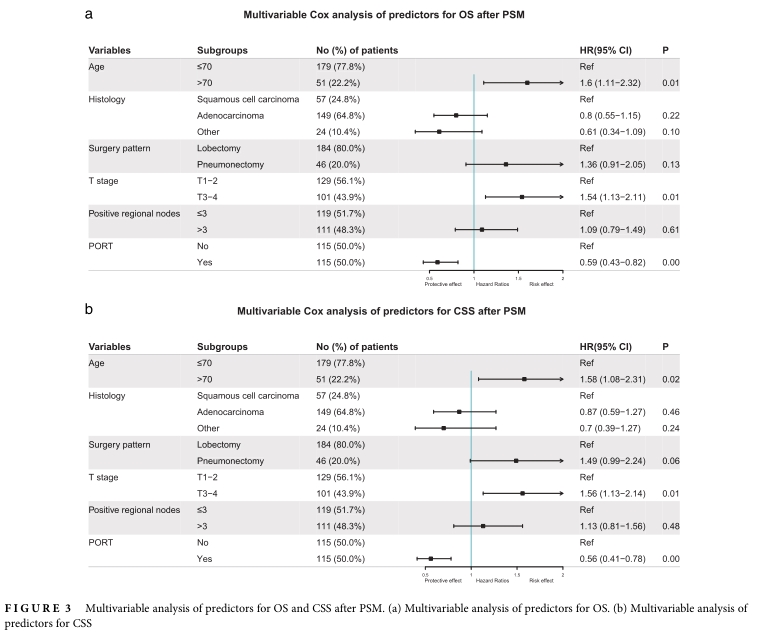
PSM后,PORT能改善大部分亚组患者的OS和CSS,其中包括:≤70岁(OS: HR = 0.60, p = 0.005;CSS: HR = 0.55, p = 0.002),诊断时为晚期患者(OS: HR = 0.38, p<0.001;CSS: HR = 0.37, p <0.001),白人(OS: HR = 0.62, p = 0.007;CSS: HR = 0.60, p = 0.005),男性(OS: HR = 0.59, p = 0.025;CSS: HR = 0.57, p = 0.02)或女性(OS: HR = 0.63, p = 0.03;CSS: HR = 0.58, p = 0.01),鳞状细胞癌(OS: HR = 0.39, p = 0.002;CSS: HR = 0.36, p = 0.002), III-IV级(OS: HR = 0.59, p = 0.007;CSS: HR = 0.54, p = 0.003),肺叶切除术(OS: HR = 0.62, p = 0.008;CSS: HR = 0.58, p = 0.003), T3-4 (OS: HR = 0.47, p<0.001;CSS: HR = 0.40, p<0.001),阳性区域淋巴结≤3个(OS: HR = 0.56, p = 0.01;CSS: HR = 0.53, p = 0.008)或>3 (OS: HR = 0.64, p = 0.04;CSS: HR = 0.59, p = 0.02)。


综上,研究表明,对于新辅助化疗术后的ypN2 NSCLC患者,术后放疗(PORT)可改善患者的OS和CSS。
原始出处:
Yongxing Bao, Xu Yang, Yu Men, et al. Postoperative radiotherapy improves survival of patients with ypN2 non-small cell lung cancer after neoadjuvant chemotherapy followed by surgery – A propensity score matching study of the Surveillance, Epidemiology, and End Results database. Thoracic Cancer. 2021;1–8. DOI: 10.1111/1759-7714.14273
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#倾向评分匹配#
30
#新辅助#
44
#术后放疗#
36
#肺癌患者#
41
#THORAC#
28
#非小细胞#
20
#非小细胞肺癌患者#
43