J Thorac Oncol:肺癌患者性别的生存差异以及预后因素对其影响
2022-03-22 yd2015 MedSci原创
研究表明,性别相关的肺癌生存差异很大程度上是由已知的预后因素所决定的,这表明有机会探索治疗偏好、选择和可及性方面的性别差异。
近期,Journal of Thoracic Oncology杂志上发表一项来自澳大利亚的研究成果,主要是基于澳大利亚人群大型队列研究,评估肺癌患者中性别差异对预后的影响。

研究纳入45 and Up研究中的肺癌患者(2006-2009年),并且随访至2015年12月。研究探索预后相关因素,并且将其分为男性和女性进行分层分析对预后影响。
在45 and Up研究的267,153名参与者中,1130名符合条件的参与者在随访期间被诊断出患有肺癌(488名女性和642名男性)。与男性相比,女性诊断时的平均年龄更小,合并症更少,受教育程度更低。女性不吸烟的可能性更大,被动吸烟的可能性更小;更有可能被诊断为腺癌,并在诊断后的6个月内接受手术。值得注意的是,性别和癌症分期之间没有显著相关性。
女性患者的中位OS为1.28年,而男性为0.77年,女性预后优于男性患者(p<0.001)。

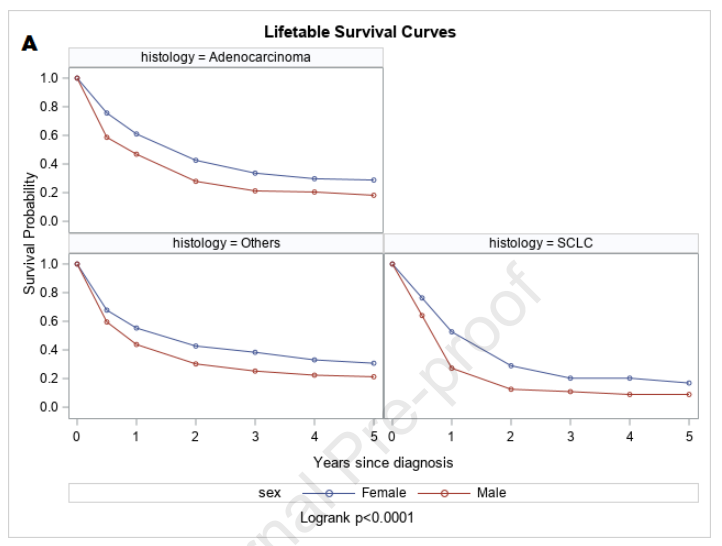
基于主要预后因素的亚组分析时,包括组织学亚型、诊断时的阶段、接受的治疗和吸烟状况,女性患者的生存长于男性患者。不管吸烟状态如何,女性腺癌患者的预后优于男性腺癌患者(logrank p=0.0009)。但是吸烟时,两组预后没有显著差异(logrank p=0.37)。然而,在诊断时,不吸烟的人比曾经吸烟的人更老(平均年龄74岁对69岁,p<0.0001),并且在调整年龄后,他们肺癌死亡的风险显著降低(HR 0.84, 95% CI 0.73-0.98)。

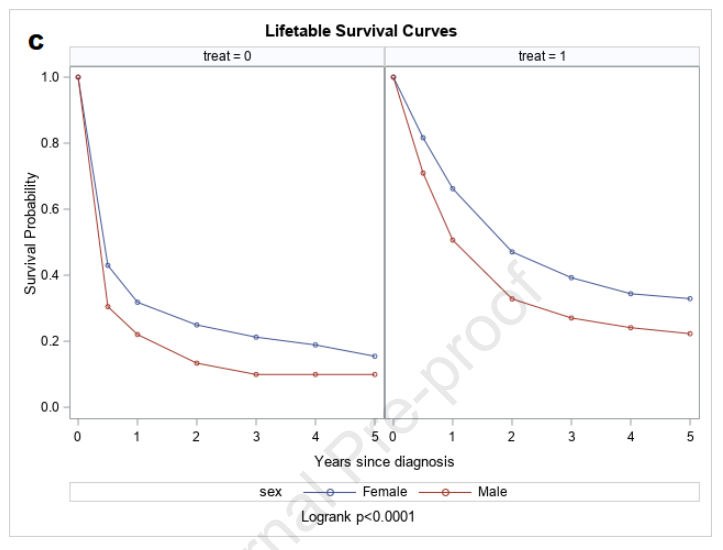

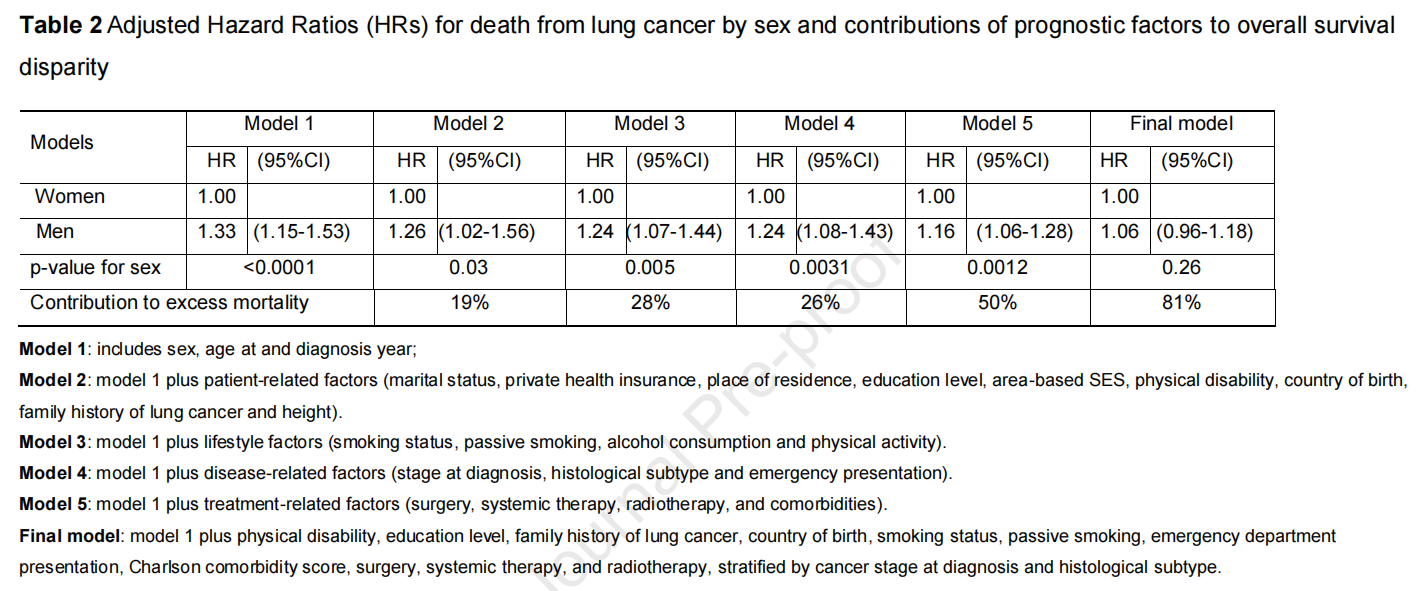
在单变量回归分析中,男性肺癌死亡风险显著高于女性(HR 1.43, 95% CI 1.25-1.64;p<0.0001)。经过最小的调整(诊断时年龄和年份),死亡的额外风险降低33% (HR 1.33, 95% CI 1.15- 1.53)。在对参与者的特征、生活方式、肿瘤或治疗相关因素进行额外的、单独的调整后,男性的额外死亡风险显著降低,但仍显著高于女性。治疗相关因素的差异解释了50%的性别生存差异。其次是生活方式和肿瘤相关因素(分别为28%和26%)。由于这些协变量域之间的相关性,域特定百分比的总和超过了100%。最终模型纳入的因素合计占男性死亡额外风险的81%,与女性差异无统计学意义(HR 1.06, 95% CI 0.96-1.18;p = 0.26)。

综上,研究表明,性别相关的肺癌生存差异很大程度上是由已知的预后因素所决定的,这表明有机会探索治疗偏好、选择和可及性方面的性别差异。
原始出处:
Yu XQ, Yap ML, Cheng ES, Ngo PJ, Vaneckova P, Karikios D, Canfell K, Weber MF. Evaluating prognostic factors for sex differences in lung cancer survival: findings from a large Australian cohort. J Thorac Oncol. 2022 Feb 3:S1556-0864(22)00085-5. doi: 10.1016/j.jtho.2022.01.016. Epub ahead of print. PMID: 35124253.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#THORAC#
42
#Oncol#
0
#肺癌患者#
39
#预后因素#
47
学习了
60