JNCCN:左侧RAS/RAF野生型(WT) 转移性结直肠癌(mCRC)患者治疗策略趋势和预后
2022-02-28 yd2015 MedSci原创
研究表明,尽管左侧RAS/RAF野生型(WT) mCRC患者一线化疗联合抗EGFR治疗改善患者预后,但是联合贝伐珠单抗仍是的常用方案。
对CALGB/SWOG 80405试验的事后分析表明,在左侧转移性大肠癌(mCRC)患者中,一线化疗时,加入抗EGFR治疗可能优于贝伐单抗。近期,来自美国的团队开展了相关研究,评估了左侧RAS/RAF野生型(WT) mCRC患者使用抗EGFR药物的趋势,并比较了最常用治疗策略的临床结果。相关结果发表在Journal of the National Comprehensive Cancer Network杂志上。
研究筛查20333例mCRC患者,纳入 1,607 (65%)患者,其中一线治疗单独化疗组有456例(28%),965例(60%)患者接受化疗加贝伐单抗,186例(12%)患者接受化疗加抗EGFR治疗。
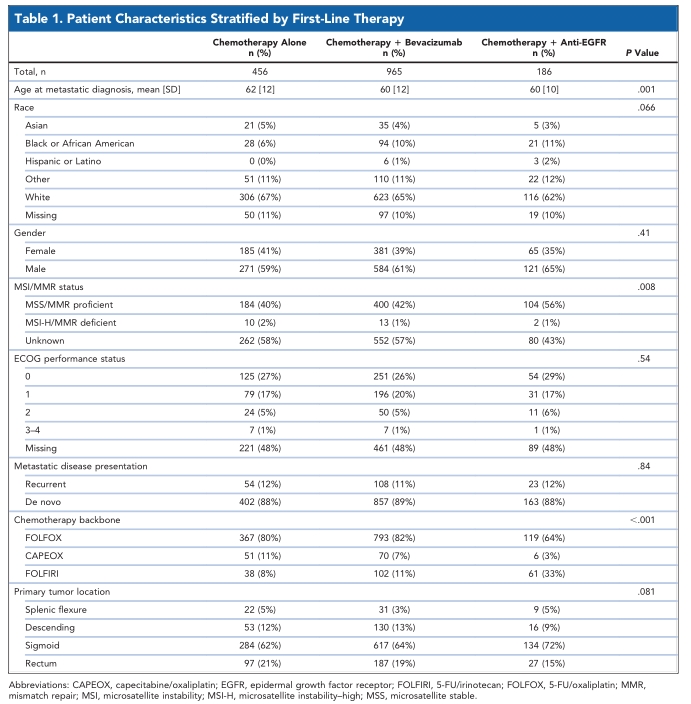
研究表明,从抗EGFR药物的使用比例从2013年的9%升高至2018年的16%,而抗VEGF药物的使用比例从63%至58%。

接受抗EGFR药物治疗患者的中位OS为42.9个月(95% CI, 36.0至未达到),而接受贝伐单抗治疗患者的中位OS为27.5个月(95% CI, 25.8-28.9),接受单独化疗患者的中位OS为27.3个月(95% CI, 24.8-32.3)。
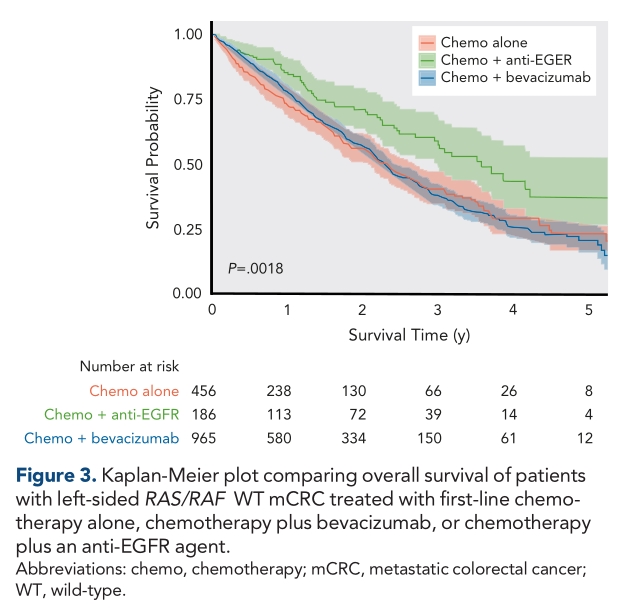
多因素分析显示,与单独化疗相比较,加入抗EGFR药物后,OS有显著改善(HR=0.52;95%CI,0.33 0.82;P=0.005),但加入贝伐单抗并不显著改善患者OS(HR=0.88;95%CI,0.68-1.14;P=0.33)。
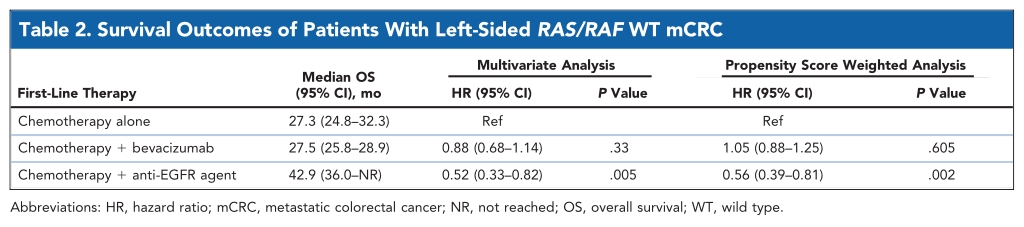
倾向评分加权生存分析也得到了相似的结果,与单独化疗相比较,加入抗EGFR药物后OS得到显著改善(HR=0.56;95%CI,0.39-0.81;P=0.002),但加入贝伐单抗并不显著改善患者OS(HR=1.05;95%CI, 0.88-1.25;P=0.605)。
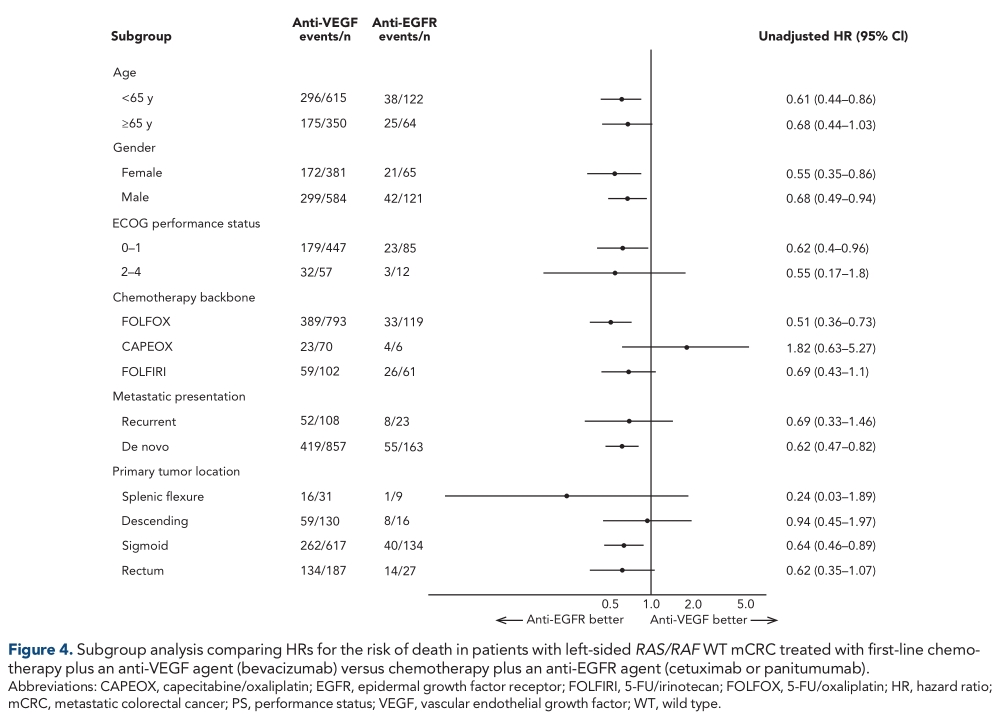
在排除未接受靶向治疗患者的单独倾向评分加权分析中,使用抗EGFR药物治疗患者的OS显著优于使用贝伐单抗治疗患者(HR=0.52;95%CI,0.37-0.73;P=0.0001)。
综上,研究表明,尽管左侧RAS/RAF野生型(WT) mCRC患者一线化疗联合抗EGFR治疗改善患者预后,但是联合贝伐珠单抗仍是的常用方案。
原始出处:
Nevala-Plagemann C, Iyengar S, Trunk AD, Pappas L, Haaland B, Garrido-Laguna I. Treatment Trends and Clinical Outcomes of Left-Sided RAS/RAF Wild-Type Metastatic Colorectal Cancer in the United States. J Natl Compr Canc Netw. 2022 Feb 4:1-8. doi: 10.6004/jnccn.2021.7079. Epub ahead of print. PMID: 35120306.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#mCRC#
57
#野生型#
50
#CRC#
45
规范化,科学化!
66
学习了
55
#NCCN#
45
#转移性#
43
#结直肠#
28