盘点:近期淋巴瘤相关指南共识一览
2016-12-04 MedSci MedSci原创
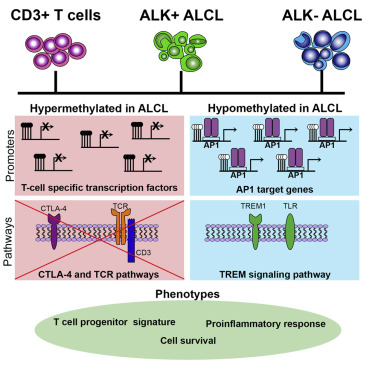
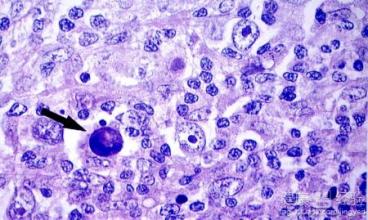
淋巴瘤是起源于淋巴造血系统的恶性肿瘤,主要表现为无痛性淋巴结肿大,肝脾肿大,全身各组织器官均可受累,伴发热、盗汗、消瘦、瘙痒等全身症状。【1】2016 NICE技术评估指南:Crizotinib用于未经治疗的间变性淋巴瘤激酶(ALK)阳性的晚期非小细胞肺癌的治疗(TA406)2016年9月28日,英国国家卫生与临床优化研究所(NICE)发布Crizotinib用于未经治疗的间变性淋巴瘤激酶(ALK
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











好资料,下载了有时间学习
2
可怕,当初得了肺结核,胸前有一肿块,去医院检查,医生当时说是淋巴瘤,检查之后确定为胸壁结核……
53
可怕,
64
好东西学习了!
0
牛
55