JAMA Oncol:紫杉醇+顺铂+卡培他滨诱导化疗可改善晚期鼻咽癌患者的生存预后
2022-04-07 Nebula MedSci原创
与采用顺铂+氟尿嘧啶方案诱导化疗相比,采用紫杉醇+顺铂+卡培他滨方案诱导治疗两个疗程可提高IVA-IVB期鼻咽癌患者的无治疗失败生存率。
鼻咽癌是我国高发的恶性肿瘤之一,发病率为耳鼻咽喉恶性肿瘤之首。鼻咽癌多对放疗具有中度敏感性,放疗是鼻咽癌的首选治疗方法。但对较高分化癌以及晚期或复发性病例,手术切除和化疗亦属于不可缺少的手段。在同步放化疗的基础上,加用诱导化疗可显著延长局部晚期鼻咽癌患者的生存期,但最佳诱导化疗方案尚不明确。
本研究旨在对比放化疗前予以紫杉醇+顺铂+卡培他滨(TPC)vs 顺铂+氟尿嘧啶(PF)诱导化疗对IVA-IVB期鼻咽癌患者预后的影响。
这是一项开放标签的、随机的3期临床试验,自2016年10月20日至2019年8月29日期间从中国的4家医院招募初治的非角化型鼻咽癌患者(18-65岁)。受试患者被随机(1:1)分成两组,接受TPC或PF方案诱导化疗,继以放化疗。主要终点是无失败生产率。次要终点包括无远处转移生存率、无局部复发生产率、总生存率、肿瘤反应和安全性。
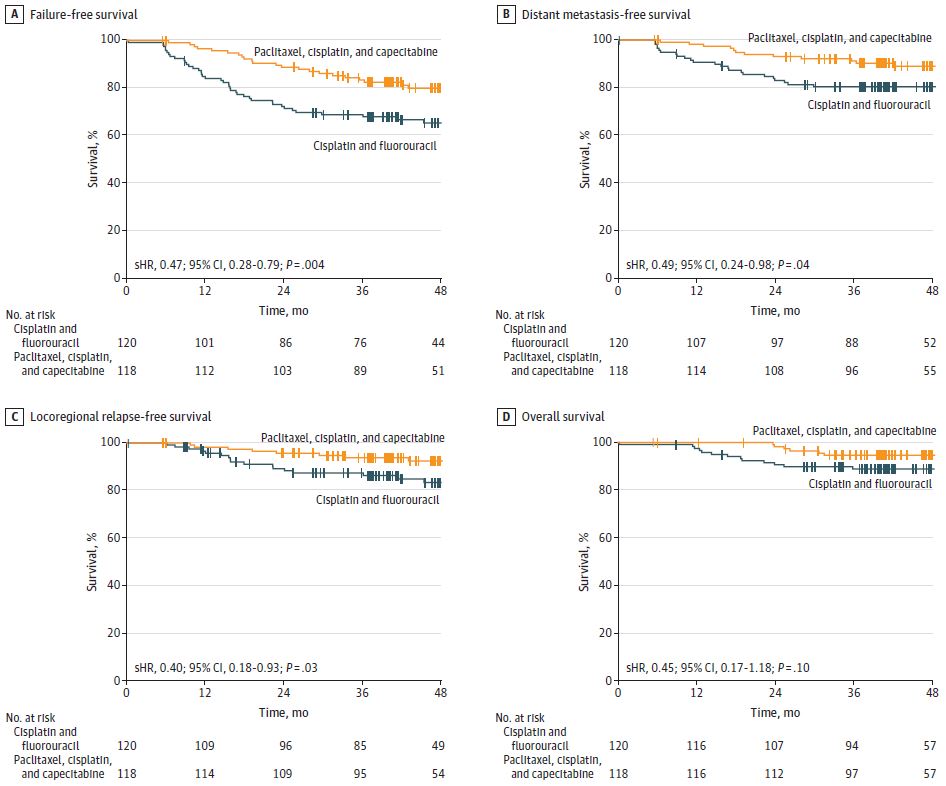
两治疗组的无治疗失败生存率(A)、无远处转移生存率(B)、无局部复发生产率(C)、总生存率(D)
共招募了238位患者(187位男性,中位年龄45岁),随机分至两组,TPC组 118位,PF组 120位。中位随访了48.4个月。TPC组和PF组的3年无治疗失败生存率分别是83.5%和68.9%(复发或死亡的分层风险比[HR] 0.47,p=0.004)。与PF方案相比,采用TPC方案诱导化疗可显著降低患者的远处转移和局部复发风险(分层HR分别是0.49[p=0.04]和0.40[p=0.03])。但是,两组的早期总生产率无显著差异(分层HR 0.45, p=0.10)。
治疗相关的急性不良事件
在TPC组中,3-4级急性不良事件和晚发型副作用的发生率分别是57.6%(n=68)和13.6%(16/118);在PF组中,3-4级急性不良事件和晚发型副作用的发生率分别是65.8%(n=79)和17.9%(21/117)。只有PF组发生了一例治疗相关死亡。
综上,该随机试验表明,与采用PF方案诱导化疗相比,采用TPC方案诱导治疗两个疗程可提高IVA-IVB期鼻咽癌患者的无治疗失败生存率,且不增加毒性。
原始出处:
Li W, Lv X, Hu D, et al. Effect of Induction Chemotherapy With Paclitaxel, Cisplatin, and Capecitabine vs Cisplatin and Fluorouracil on Failure-Free Survival for Patients With Stage IVA to IVB Nasopharyngeal Carcinoma: A Multicenter Phase 3 Randomized Clinical Trial. JAMA Oncol. Published online March 24, 2022. doi:10.1001/jamaoncol.2022.0122.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#生存预后#
37
#Oncol#
35
#铂#
41
#卡培他滨#
53
#诱导化疗#
41