JAHA:中国≥40岁居民36.2%颈动脉粥样硬化
2018-04-09 卢芳 中国循环杂志
“中国卒中防治工程“项目组分析了84880名中国居民的颈动脉超声数据,发现中国≥40岁居民中有36.2%颈动脉粥样硬化。
“中国卒中防治工程“项目组分析了84880名中国居民的颈动脉超声数据,发现中国≥40岁居民中有36.2%颈动脉粥样硬化。
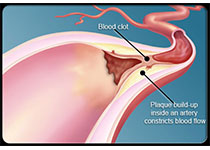
颈动脉粥样硬化的定义是颈动脉内膜中层厚度(IMT)增厚≥1 mm或存在斑块。研究排除了已接受颈动脉内膜切除术、支架以及有卒中和冠心病的居民。
研究中约26.5%居民IMT增加,13.9%居民存在斑块。
这个数据远远低于中国慢病前瞻性研究(CKB)31%的斑块患病率。但CKB研究纳入了有卒中(5.4%)和冠心病(7.5%)的患者。
农村居民的颈动脉粥样硬化患病率为41.6%,高于城市居民的30.8%。
研究者认为这与受教育水平低,以及因经济状况欠佳、医疗资源不均衡等有关。
研究还显示,IMT<1 mm的受试者中有8.7%的人颈动脉存在单个或多个粥样斑块。
男性颈动脉粥样硬化比女性更常见。可能是因为男性有更多不良生活习惯,比如很多人都是烟民,很多人都喜欢喝酒。
比如,吸烟(包-年)与颈动脉中膜厚度、粥样斑块形成呈剂量依赖关系,
研究中男性占46.4%,平均年龄60.7岁。
原始出处:
Wang X, et al. Carotid Atherosclerosis Detected by Ultrasonography: A National Cross-Sectional Study. J Am Heart Assoc. 2018 Apr 5;7(8).
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#粥样硬化#
23
#颈动脉#
19
#AHA#
24
#颈动脉粥样硬化#
37
一起学习学习
56