Clin Cancer Res:III期临床研究CATNON表明IDH野生型的胶质母细胞瘤中,在放疗的基础上加用替莫唑胺并不能改善患者的预后
2022-03-14 网络 网络
研究表明,在IDH野生型的胶质母细胞瘤中,在放疗的基础上加用替莫唑胺并不能改善患者的预后。
近期,CLINICAL CANCER RESEARCH杂志上发表了一项III期临床研究CATNON (NCT00626990)的事后分析结果,主要是评估在IDH野生型的胶质母细胞瘤中,在放疗的基础上加用替莫唑胺是否提高患者的疗效。
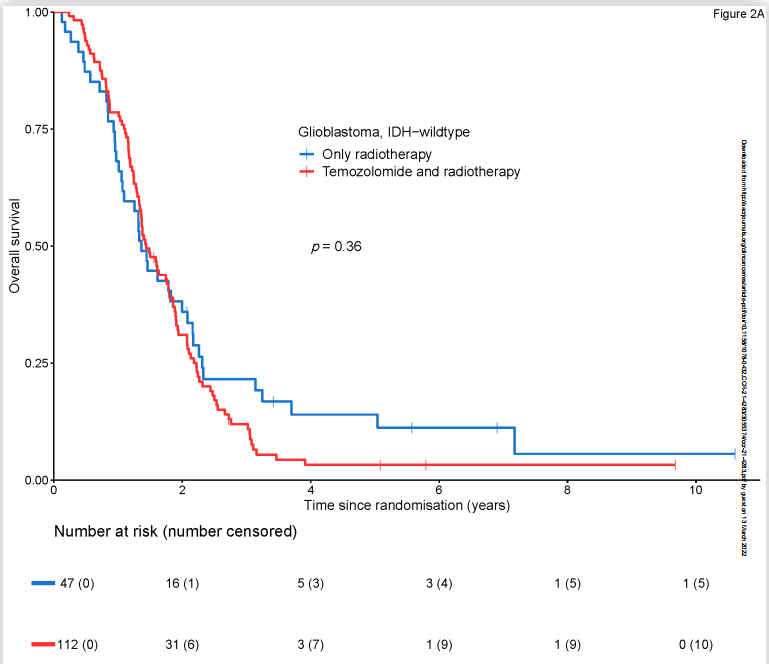
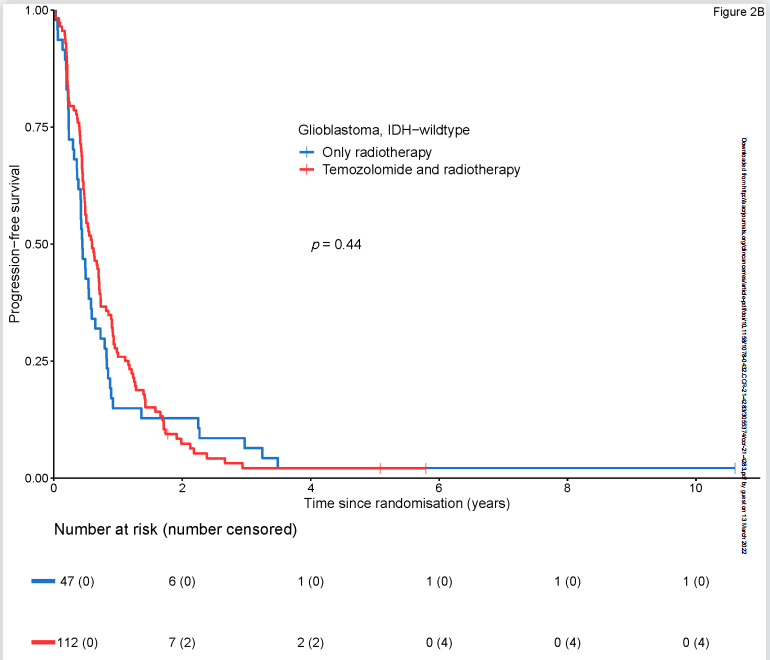
在参与CATNON研究的751例患者中,有670例具有完全分子特征的肿瘤。其中159例符合世卫组织2021年IDH野生型胶质母细胞瘤分子标准。在这些患者中,47例(29.6%) 仅接受放疗,112例(70.4%) 接受放疗和替莫唑胺联合治疗。两组的特征类似,而联合组中MGMT启动子非甲基化肿瘤比例趋于更高(p=0.066)。
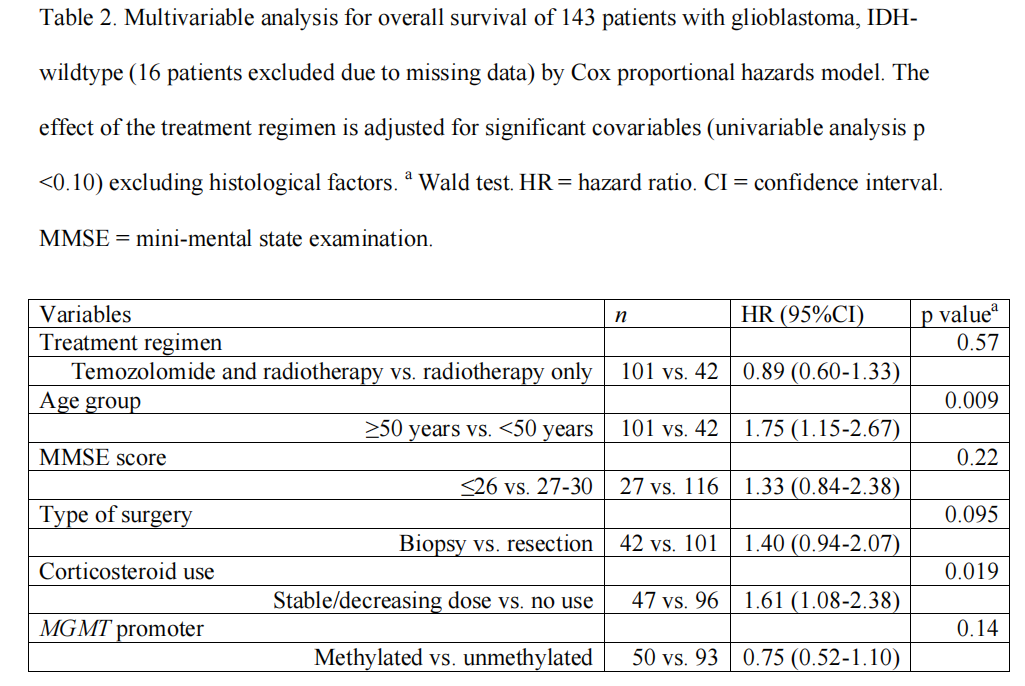
IDH野生型的胶质母细胞瘤患者的中位总生存期(OS)为1.4年(95% CI 1.3-1.8年),中位无进展生存期(PFS)为0.5年(95% CI 0.5-0.7年)。加入替莫唑胺对总生存期(HR=1.19, 95% CI 0.82-1.71)和无进展生存期(HR=0.87, 95% CI 0.61-1.24)均没有增加影响。
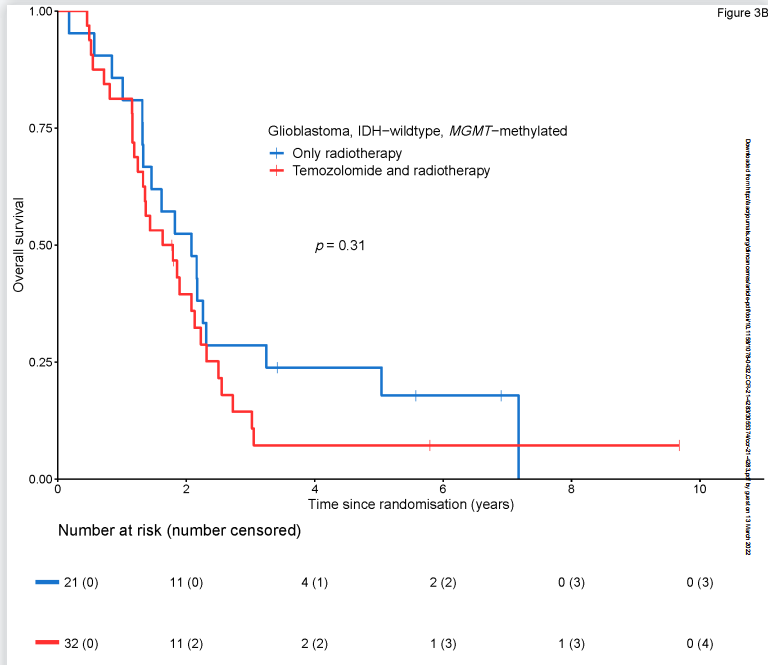
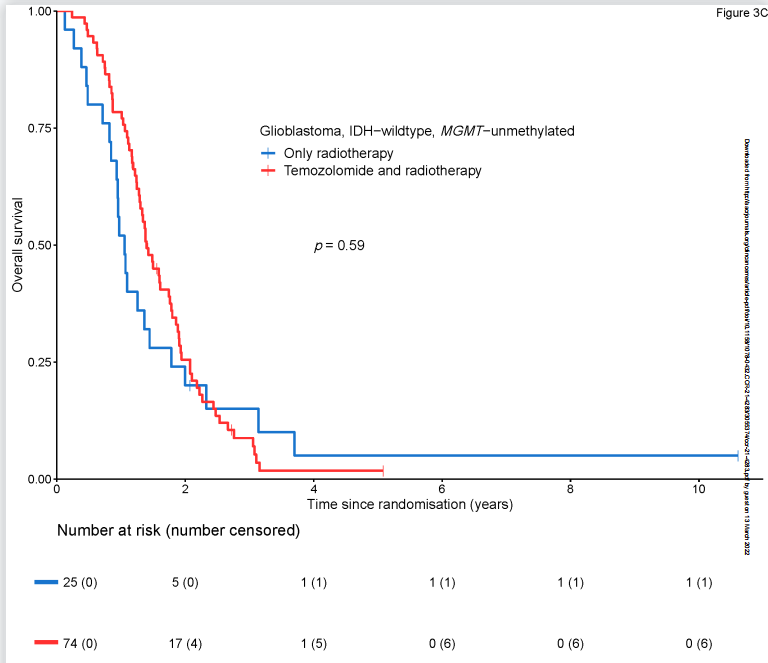
152例患者中,MGMT启动子甲基化有53例(34.9%),MGMT非甲基化有99例(65.1%)。MGMT甲基化肿瘤患者的总生存期优于非甲基化患者(HR=0.65, 95% CI 0.45-0.92); MGMT甲基化肿瘤组的中位总生存期为1.8年(95% CI 1.4-2.2年),MGMT非甲基化肿瘤组的中位总生存期为1.4年(95% CI 1.2-1.6年)。MGMT启动子甲基化对无进展生存期无影响(HR 0.95, 95%CI 0.68-1.34),MGMT甲基化肿瘤组的中位PFS为0.5年(95% CI 0.4 -0.8年),而MGMT非甲基化肿瘤组的中位PFS也是0.5年(95% CI 0.5-0.7年)。
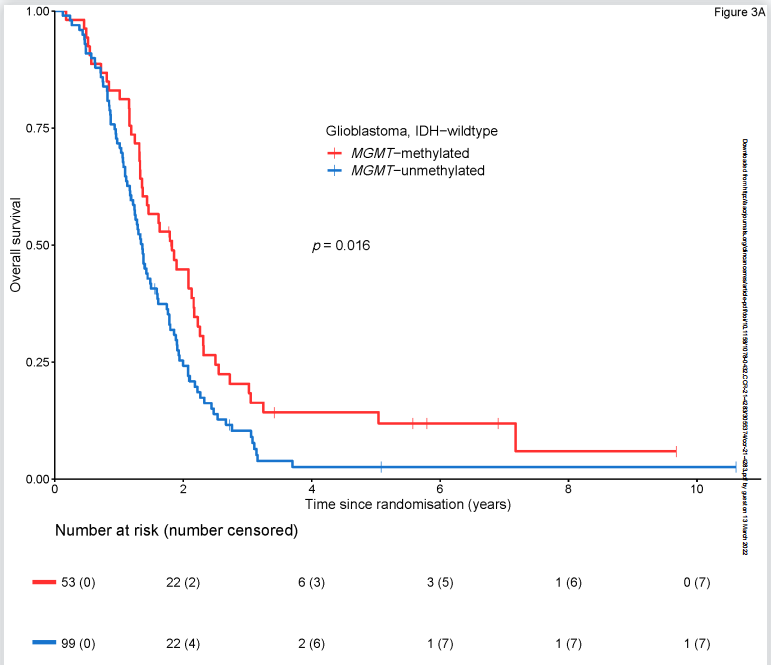
同样,在MGMT启动子甲基化肿瘤组(HR 1.36, 95% CI 0.75-2.48)和MGMT非甲基化肿瘤组(HR 0.88, 95% CI 0.54-1.42)患者中,加入替莫唑胺均未检测到生存益处。
校正多因素的分析中,替莫唑胺的加入并不能较单独放疗改善患者的总生存期(HR=1.03, 95% CI 0.69-1.53)和无进展生存期(HR=0.79, 95% CI 0.55-1.13)。
综上,研究表明,在IDH野生型的胶质母细胞瘤中,在放疗的基础上加用替莫唑胺并不能改善患者的预后。
原始出处:
Tesileanu CMS, Sanson M, Wick W, Brandes AA, et al. Temozolomide and radiotherapy versus radiotherapy alone in patients with glioblastoma, IDH-wildtype: post-hoc analysis of the EORTC randomized phase 3 CATNON trial. Clin Cancer Res. 2022 Mar 11:clincanres.4283.2021. doi: 10.1158/1078-0432.CCR-21-4283. Epub ahead of print. PMID: 35275197.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#II期临床研究#
49
#野生型#
47
#I期临床#
49
#母细胞瘤#
52
#胶质母细胞#
29
#III期临床研究#
36
#III#
27
#细胞瘤#
31
#II期临床#
32
#III期#
35