英国《自然—医学》期刊的研究显示,一个美国团队通过改变小鼠肠道菌群特性来调控免疫系统,成功降低了它们中风后脑部遭受的损伤。未来如能证明这种机制适用于人类,或许能开发出针对中风等疾病的新疗法。
人体肠道内寄生着大量细菌,它们能影响体重和消化能力、抵御感染和自体免疫疾病的患病风险。
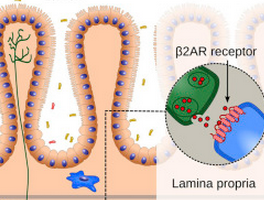
美国韦尔·康奈尔医学院学者领衔的团队利用动物模型进行的实验显示,肠道菌群具有调节与炎症相关免疫细胞的作用,这些免疫细胞在小鼠出现中风后会从肠道转移到脑部。
实验中,团队让一部分小鼠摄入多种抗生素,另一部分则不服用任何药物。两周后,他们在所有小鼠身上诱发中风。结果发现服用抗生素的小鼠比对照组小鼠中风程度低约60%。
据研究人员介绍,这主要是因为小鼠服用抗生素后,肠道菌群发生变化,打破了肠道中引起炎症和对抗炎症的两种免疫细胞间的平衡,后者数量上升,最终抑制了那些引起炎症的免疫细胞在小鼠中风后转移到它们脑部,脑部所受损伤也因此降低。
尽管还需通过进一步研究来验证这种机制是否存在于人类肠道内,但研究作者之一、韦尔·康奈尔医学院学者约瑟夫·安拉特说,这项实验展示了脑部与肠道间存在的联系,肠道菌群能够影响中风程度,这或许能让研究人员重新审视预防和治疗中风的方法,比如通过改变病患的饮食来改善他们肠道菌群特性。
小编推荐一个会议:,超级火爆,牛人会集!接收新信息,明天基金申请就靠它了!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#病情#
29
#Nat#
21
#肠道菌#
21
#变性#
25
#Med#
25
肠道菌群的相关研究很火热呀,学习了
146
这有点蝴蝶效应的味道!
137
学习了,很好
102
…………
101
哲学上讲事物之间是普遍联系的,没有做不到,只有想不到。关键是影响力有多大。
129