European Radiology:前庭神经鞘瘤伽GKRS术前的动态增强MRI的反应预测
2022-06-03 shaosai MedSci原创
动态增强(DCE)MRI可以根据定量的药代动力学参数提供组织通透性和血管生成的信息,已应用于临床的多个领域。
 伽玛刀放射外科手术(GKRS)是治疗中小型前庭神经鞘瘤(VS)的一种成熟的治疗方案,可有效控制肿瘤的生长。新阶段,评估GKRS后治疗反应的唯一方法是进行长期随访成像。此外,GKRS治疗后肿瘤大小的一过性增加是一个众所周知的现象,这使得评估治疗反应更加困难。
伽玛刀放射外科手术(GKRS)是治疗中小型前庭神经鞘瘤(VS)的一种成熟的治疗方案,可有效控制肿瘤的生长。新阶段,评估GKRS后治疗反应的唯一方法是进行长期随访成像。此外,GKRS治疗后肿瘤大小的一过性增加是一个众所周知的现象,这使得评估治疗反应更加困难。
动态增强(DCE)MRI可以根据定量的药代动力学参数提供组织通透性和血管生成的信息,已应用于临床的多个领域。然而,对VS的DCE-MRI研究却很少。据我们所知,没有研究评估使用DCE-MRI来预测GKRS后的治疗反应。
近日,发表在European Radiology杂志的一项研究探讨了治疗前DCE-MRI参数对散发性VS进行GKRS后肿瘤反应的预测作用,为临床制定个性化治疗方案提供了有价值的参考。
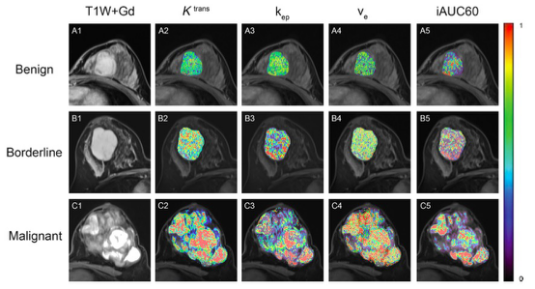
本项单中心前瞻性研究在2017年4月至2019年2月期间招募了研究参与者,并在GKRS前对DCE-MRI衍生的参数进行了体积测量。在随访的MRI中测量肿瘤体积。根据20%或更多的肿瘤体积缩小,比较有反应者和无反应者的药代动力学参数。进行逐步的多变量逻辑回归分析,并通过受试者工作特征曲线分析评估DCE-MRI参数对预测肿瘤反应的诊断性能。
最终,共35名参与者(21名女性,52±12岁)被纳入研究。有22名(62.9%)有反应者,平均随访时间为30.2±5.7个月。Ktrans(0.036 min-1 vs. 0.057 min-1,p = .008)和90s内时间浓度曲线下的初始面积(IAUC90)(84.4 vs. 143.6,p = .003)显示出反应者和无反应者之间的显著差异。Ktrans(OR = 0.96,p = .021)和IAUC90(OR = 0.97,p = .004)是每个多变量模型中的重要区分变量,与临床变量一起用于预测肿瘤反应。Ktrans预测肿瘤反应的敏感性为81.8%、特异性为69.2%,IAUC90的敏感性为100%、特异性为53.8%。
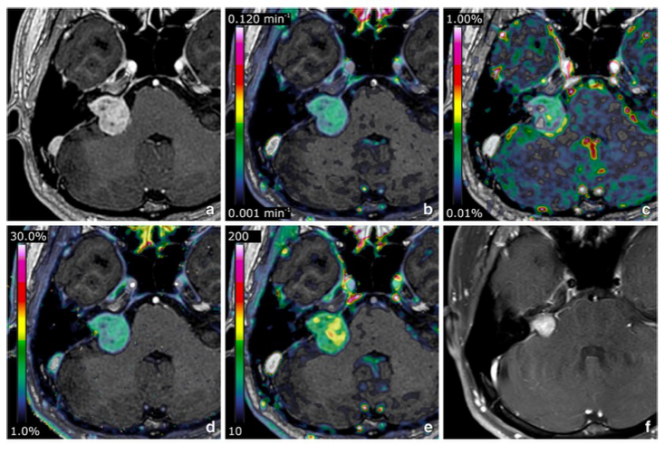
图 35岁男性,诊断为右前庭神经鞘瘤,并接受了伽玛刀放射外科治疗。显示了基线增强T1加权图像(a)和叠加的Ktrans(b)、vp(c)、ve(d)和IAUC90(e)maps(TR,8.1ms;TE,3.2ms)。整个肿瘤的基线平均Ktrans值为0.027 min-1,平均IAUC90为91.3。在GKRS 32个月后的随访MRI上(f),肿瘤显示出74.5%的体积缩小(TR,593 ms;TE 6.6 ms)
本研究结果表明,DCE-MRI衍生的Ktrans和IAUC90可作为GKRS后VS肿瘤反应的预测因素。考虑到对肿瘤反应的敏感性和相对较短的随访期,DCE-MRI对相对早期的肿瘤反应具有预测价值。
原文出处:
Inpyeong Hwang,Seung Hong Choi,Jin Wook Kim,et al.Response prediction of vestibular schwannoma after gamma-knife radiosurgery using pretreatment dynamic contrast-enhanced MRI: a prospective study.DOI:10.1007/s00330-021-08517-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PE#
47
#前庭神经#
45
#动态增强MRI#
45
#神经鞘瘤#
66