Int Arch Allergy Immunol:触变鼻用凝胶对鼻症状和炎症生物标记影响研究
2020-04-21 AlexYang MedSci原创
无药粘性鼻腔应用在季节过敏性鼻炎(SAR)中能够减少鼻症状。Nascum®-Plus (NP)是一种商业化的触变胶体,已经设计用于减少鼻粘膜的干燥和疼痛,并预防小颗粒的吸入。最近,有研究人员评
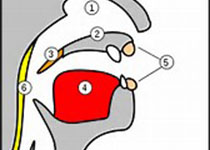
无药粘性鼻腔应用在季节过敏性鼻炎(SAR)中能够减少鼻症状。Nascum®-Plus (NP)是一种商业化的触变胶体,已经设计用于减少鼻粘膜的干燥和疼痛,并预防小颗粒的吸入。最近,有研究人员评估了单剂量的NP在过敏原挑战(ACC)期间治疗鼻症状和分泌的效果情况。更多的是,研究人员还测量了上述治疗对生物标记和过敏途径的免疫细胞的影响情况。
研究是一个开放标签、交叉、序列随机和单中心随机试验,包括了18名SAR成年人。对Dactylis glomerata花粉显示阳性皮刺测试结果的患者接受NP治疗,否则不进行治疗,共进行了2次4小时的ACC,间隔为3周。在第1天,9名受试者进行4小时的挑战并进行治疗,另外9名没有进行治疗,在第22天反之亦然。研究发现,NP能够显著的减轻鼻症状(p<0.001),并使鼻分泌减到最轻(p=0.047),而在鼻分泌液中没有观察到对生物标记和免疫细胞的明显影响。因此,治疗是安全的并具有良好的耐受性。
最后,研究人员指出,NP鼻凝胶建立的屏障可以安全的在过敏性鼻炎患者中使用。它能够减少过敏性鼻症状和分泌,但是单剂量的使用并不影响局部炎症生物标记。
原始出处:
Struß N, Badorrek P, Mattern C et al. The Effect of a Thixotropic Nasal Gel on Nasal Symptoms and Inflammatory Biomarkers in Seasonal Allergic Rhinitis. Int Arch Allergy Immunol. 07 April 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#鼻症状#
39
#ALL#
25
#生物标记#
0
#凝胶#
30
好
83
好
71