Pediatrics:为什么我们不能根除先天梅毒?
2021-10-24 医路坦克 MedSci原创
在我们能够解决社会上持续未能控制梅毒的问题之前,我们不能根除CS,但我们可以通过识别和及时治疗所有患有梅毒的孕妇,以及在没有症状的CS婴儿出现症状之前对其进行治疗,来降低CS的风险。
先天性梅毒(CS)的流行有增无减,尽管循证医学建议对所有孕妇进行筛查,并提供高效的青霉素疗法,但CS病例在美国继续增加。
2019年全美CS发病率为每10万例新生儿中有48.5例,比2018年增加41.4%,比2015年增加291.1%。有94例梅毒产儿死亡和34例与CS有关的婴儿死亡。在怀孕期间和新生儿期之后没有诊断和治疗梅毒或延误治疗可能会导致更严重的疾病和终生发病率。
在本期“儿科”杂志中,Kimball等人提醒我们注意照顾儿童的医疗保健专业人员面临的另一个挑战:新生儿出院后被诊断为CS的婴儿数量不断增加,这在很大程度上是因为仍然未能诊断和迅速处理患有梅毒的孕妇及其新生儿。
2019年,最常见的错失机会是:尽管得到及时诊断,但没有提供足够的孕产妇梅毒治疗(40.2%),缺乏最佳的产前护理,随后缺乏推荐的检测(36.3%)。还发现的还有妊娠期间血清转换晚,尽管接受了充分的产前护理,但没有进行梅毒检测,以及产妇治疗失败。孕妇可能在分娩时感染梅毒,并在她进行可检测的血清学反应之前将梅毒螺旋体传染给胎儿。在这种情况下,儿科卫生保健专业人员需要意识到稍后出现的CS。
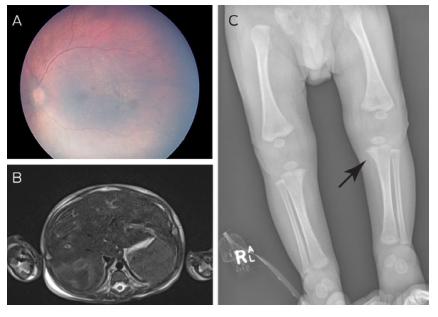
Kimball等人报道,从2014年到2018年,在3834名被诊断为CS的婴儿中,84名(2.2%)被诊断为超过新生儿期,其中68名(80.9%)有症状。确诊时的中位年龄为67天。虽然大多数妇女接受了产前护理,但在出院前未能发现患有CS的婴儿与两个关键因素有关:未充分按照指南进行筛查和治疗,以及未能确定推荐在怀孕28周和分娩时重复筛查的妇女。42%的母亲在分娩后才被诊断出患有梅毒,其中超过一半的母亲是在婴儿被诊断出梅毒后才被确诊的。雪上加霜的是,9%的婴儿没有接受推荐的CS治疗。这些婴儿的延迟诊断导致了症状性疾病的发展,使他们更容易出现更严重的临床表现,并有可能出现晚期和永久性的后遗症。
在最近的一项研究中,研究人员发现,只有50%的梅毒孕妇报告了梅毒暴露的已知风险因素,这突显了使用基于风险的策略来识别在怀孕28周和分娩时需要重复血清学测试的个人的局限性。在怀孕期间对所有孕妇进行3次检测:第一次产前检查,怀孕28周以及分娩时。出生时患有CS的婴儿数量不断增加,这是一种公共卫生紧急情况。及时治疗患有梅毒的孕妇,了解母亲在分娩时的血清学状况,对于识别有CS风险的婴儿或患有CS的婴儿至关重要。在产房里,梅毒的快速医疗检测可能会有帮助。
遗憾的是,在我们能够解决社会上持续未能控制梅毒的问题之前,我们不能根除CS,但我们可以通过识别和及时治疗所有患有梅毒的孕妇,以及在没有症状的CS婴儿出现症状之前对其进行治疗,来降低CS的风险。
文献来源:Bocchini JA, Vanchiere JA, Sánchez PJ,Why Can't We Eradicate Congenital Syphilis?Pediatrics 2021 Aug 31;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PE#
28
#Pediatric#
42
#根除#
30
#DIA#
31
梅毒,母婴传播
47