Cancer Res:纤蛋白-3激活Notch通路促进神经胶质细胞瘤恶性
2012-06-17 bo 生物谷
6月4日Cancer Research杂志在线报道了纤蛋白-3促进肿瘤侵袭的机制研究新发现。纤蛋白-3是一种不存在于正常大脑,而在神经胶质细胞瘤中显著上调的基质蛋白。其促进肿瘤侵袭的机制不明。恶性神经胶质细胞瘤是高侵袭性、化疗抵抗性脑瘤,预后极差。浸润性神经胶质细胞瘤细胞是复发的主要来源。针对触发侵袭和化疗抵抗的可溶性因子,也许可以对这类癌细胞有显著的抑制效果。 这项研究揭示:纤蛋白-3作为No
6月4日Cancer Research杂志在线报道了纤蛋白-3促进肿瘤侵袭的机制研究新发现。纤蛋白-3是一种不存在于正常大脑,而在神经胶质细胞瘤中显著上调的基质蛋白。其促进肿瘤侵袭的机制不明。恶性神经胶质细胞瘤是高侵袭性、化疗抵抗性脑瘤,预后极差。浸润性神经胶质细胞瘤细胞是复发的主要来源。针对触发侵袭和化疗抵抗的可溶性因子,也许可以对这类癌细胞有显著的抑制效果。
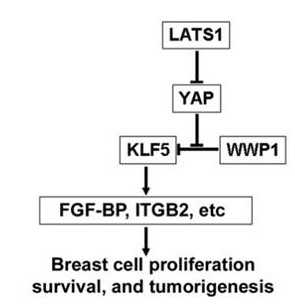
这项研究揭示:纤蛋白-3作为Notch信号通路的一种新的可溶性激活蛋白,对抗Notch的自分泌抑制物DDL3,并以不依赖于Notch的方式促进肿瘤细胞的生存和侵袭。运用可诱导下调策略,研究者发现纤蛋白-3的可控性下调降低了Notch通路活性,进而导致细胞凋亡增加,胶质母细胞瘤启动细胞的自我更新性下降,以及颅内癌细胞生长和扩散的抑制。此外,纤蛋白-3表达还与Notch依赖的基因表达水平相关,而且是患者来源神经胶质细胞瘤标本中Notch通路激活的标志。
这些发现再次证明,肿瘤细胞外基质通过激活Notch通路,调节神经胶质细胞瘤侵袭和对抗凋亡中发挥重要作用。尤为重要的是,研究者在肿瘤模型中,发现了一种非经典的Notch通路可溶性激活因子。他们还阐明了,在肿瘤微环境中Notch通路是如何肿瘤特异性因子所下调的。(生物谷bioon.com)

doi:10.1016/j.cell.2011.10.017
PMC:
PMID:
Fibulin-3 promotes glioma growth and resistance through a novel paracrine regulation of Notch signaling
Bin Hu1, Mohan S Nandhu1, Hosung Sim1, Paula A Agudelo-Garcia1, Joshua C Saldivar1, Claire E Dolan1, Maria E Mora1, Gerard J. Nuovo2, Susan E Cole3, and Mariano S Viapiano1,*
Malignant gliomas are highly invasive and chemoresistant brain tumors with extremely poor prognosis. Targeting of the soluble factors that trigger invasion and resistance therefore could have a significant impact against the infiltrative glioma cells that are a major source of recurrence. Fibulin-3 is a matrix protein that is absent in normal brain but upregulated in gliomas and promotes tumor invasion by unknown mechanisms. Here, we show that fibulin-3 is a novel soluble activator of Notch signaling that antagonizes DLL3, an autocrine inhibitor of Notch, and promotes tumor cell survival and invasion in a Notch-dependent manner. Using a strategy for inducible knockdown, we found that controlled downregulation of fibulin-3 reduced Notch signaling and led to increased apoptosis, reduced self-renewal of glioblastoma initiating cells, and impaired growth and dispersion of intracranial tumors. In addition, fibulin-3 expression correlated with expression levels of Notch-dependent genes and was a marker of Notch activation in patient-derived glioma samples. These findings underscore a major role for the tumor extracellular matrix in regulating glioma invasion and resistance to apoptosis via activation of the key Notch pathway. More importantly, this work describes a non-canonical, soluble activator of Notch in a cancer model and demonstrates how Notch signaling can be reduced by targeting tumor-specific accessible molecules in the tumor microenvironment.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#神经胶质细胞#
34
#Notch#
25
#胶质细胞#
35
#细胞瘤#
37
#OTC#
29