专访|梁景平:牙髓坏死也能“把根留住”,根管治疗拯救坏牙
2017-07-07 肖蓓 澎湃新闻
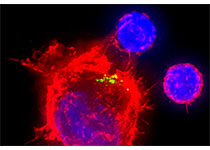
牙疼不是病,疼起来真要命。对于牙髓坏死和根尖周组织感染的严重龋病患者来说,钻心一般的疼痛,让很多人招架不住,只得将牙齿连根拔起,安装义齿。而随着根管治疗术的不断发展,尤其是显微根管治疗成功率明显提高,牙髓坏死的牙齿,通过治疗可以把根留住,从而恢复牙齿的形态和功能。上海交通大学医学院附属第九人民医院牙体牙髓科主任梁景平教授,从事根管治疗近四十余年,在镍钛根管预备及弯曲根管治疗和显微根管治疗方面积累了
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#牙髓#
46
#专访#
30
#坏死#
31
#根管#
36
非常好的文章,学习了,很受益
61
非常好,全面,实用!
50