新型口服抗凝药预防亚洲人群非瓣膜房颤患者卒中的优势
2015-07-06 张玉生 暨南大学附属第一医院 天坛国际脑血管病会议
首先张玉生教授介绍了亚洲AF患者的特点和传统抗栓治疗。根据流行病学调查研究显示亚洲AF疾病负荷将持续增加,尤其是中国,到2050年中国男性房颤患者将达到250万,女性房颤患者将达到310万。多个大型RCT研究(如RE-LY、ROCKET、ARISTOTLE、ENGAGE)或注册研究(如REALISE、RELY、RECORD)结果均显示亚洲AF患者
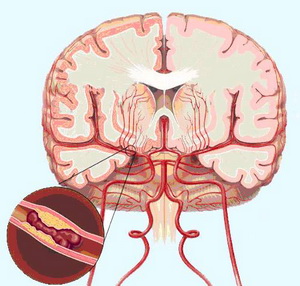
首先张玉生教授介绍了亚洲AF患者的特点和传统抗栓治疗。根据流行病学调查研究显示亚洲AF疾病负荷将持续增加,尤其是中国,到2050年中国男性房颤患者将达到250万,女性房颤患者将达到310万。多个大型RCT研究(如RE-LY、ROCKET、ARISTOTLE、ENGAGE)或注册研究(如REALISE、RELY、RECORD)结果均显示亚洲AF患者合并卒中/ TIA的比例均高于非亚洲人群。另外对36项人群研究的荟萃分析,纳入了21个国家、9 151 929例人群,有8145例颅内出血患者。该分析提示亚洲人群基线颅内出血的发生风险更高,基本上是白人的两倍以上。
可见亚洲AF患者特点:
• AF疾病负荷沉重
• 卒中和栓塞风险更高
• 颅内出血风险更高
关于AF患者抗栓治疗,2007年一项Meta分析发现,华法林直接与阿司匹林对比显示华法林降低卒中风险达39%,提示AF患者卒中预防抗凝治疗显著优于抗血小板治疗。而关于亚洲人群的一项来自香港的研究纳入了9727例非瓣膜AF患者,随访3年以上,结果显示抗凝治疗效果>抗血小板>不抗栓。胡大一教授主持的大陆一项研究纳入了非瓣膜AF患者704例,华法林预防中国大陆AF患者缺血性卒中的疗效显著优于阿司匹林。关于AF患者口服抗凝治疗普及情况,RE-LY前瞻性AF登记研究,纳入46个国家,15,400例急诊AF患者,统计CHADS2≥2的AF患者使用华法林比例,结果北美华法林使用比例60%以上,西欧、中欧洲均在50%以上,而中国仅为10%左右,明显较低。国内一项调查研究显示中国大陆AF患者抗凝治疗率仅为14.3%,明显不足。关于AF患者对华法林治疗的反应,4个NOAC AF Ⅲ期临床研究显示亚洲AF患者华法林组缺血性事件、出血事件发生率均高于非亚洲人群;多项研究提示亚洲AF患者国际标准化比值 (INR)易波动,削弱了华法林的疗效和安全性,无论在临床试验还是真实世界中,亚洲AF患者服用华法林期间INR达标率均较非亚洲患者差。
可见亚洲AF患者治疗现状:
• 抗凝治疗显著优于抗血小板治疗
• 华法林治疗率低
• 华法林治疗后INR达标率低
• 华法林的治疗反应不理想
因此亚洲AF患者亟需新型口服抗凝药:
• 疗效不劣于或优于华法林
• 安全性优于华法林
• 无需监测、无治疗窗限制
非瓣膜病AF患者新型口服抗凝剂(NOAC):
• 凝血酶抑制剂:达比加群(dabigatran) RE-LY研究
• Xa因子抑制剂:利伐沙班(rivaroxaban) ROCKET-AF研究,阿哌沙班(apixaban) AVERROES和ARISTOTLE研究,依度沙班(edoxaban) ENGAGE-AF研究
荟萃分析显示NOAC在亚洲AF患者预防卒中/全身性栓塞的疗效与总体人群结果一致,且NOAC在亚洲AF患者出血风险更小。
国内外指南/专家共识对NOAC预防非瓣膜AF患者卒中的推荐:
2014 AHA/ASA卒中/短暂性脑缺血发作预防指南
• 对于阵发性或持续性非瓣膜性AF患者,均有必要使用维生素K拮抗剂(Ⅰ类,A级)、 阿哌沙班(Ⅰ类,A级)和达比加群(Ⅰ类,B级)预防卒中复发。应根据危险因素、价格、耐受性、患者偏好、潜在的药物相互作用及其他临床特点,包括肾功能以及INR达标时程(已服VKA患者),进行个体化抗凝药的选择。
• 非瓣膜性房颤患者使用利伐沙班预防复发性卒中是合理的(Ⅱa类,B级)。
• 对于所有缺血性卒中或TIA患者,都不推荐口服抗凝药(华法林或NOAC)与抗血小板药联合治疗,但对合并明显临床冠状动脉疾病(CAD)的患者,尤其是有急性冠状动脉综合征或支架置入术患者,这种联合治疗是合理的(Ⅱb类,C级)。
• 对于伴有AF的急性缺血性卒中或TIA患者,如果不能接受口服抗凝药,推荐单独使用阿司匹林治疗(Ⅰ类,A级)。与阿司匹林单药治疗相比,阿司匹林联用氯吡格雷治疗可能是合理的(Ⅱb类,B级)。
2014缺血性卒中/TIA患者合并AF抗栓治疗中国专家共识
• 伴AF的缺血性卒中/TIA患者,推荐长期口服抗凝剂治疗(I级推荐,A级证据)。抗凝剂可选择华法林(I级推荐,A级证据) 或新型口服抗凝剂(达比加群、利伐沙班或阿哌沙班;I级推荐,B级证据)。新型口服抗凝剂疗效不劣于或优于华法林,安全性更高。
• 伴AF的缺血性卒中/TIA患者口服华法林抗凝过程中,应定期监测INR并调整其剂量,INR靶目标值为2.0~3.0 (I级推荐,A级证据)。
• 对口服抗凝剂有禁忌、不依从或没有条件使用者,推荐使用抗血小板治疗(Ⅰ级推荐,A级证据)。氯吡格雷联合阿司匹林的疗效优于单用阿司匹林,但增加大出血风险,有一定的净效益 (II级推荐,B级证据)。
• 推荐对所有需抗栓治疗的患者使用HAS-BLED评分等工具评估出血危险(I级推荐,B级证据)。HAS-BLED评分大于3分者仍可因抗栓而获益,但应积极控制出血的危险因素,严密监测,并与患者做好沟通。
2014中国缺血性卒中和TIA二级预防指南
• 对伴有AF(包括阵发性)的缺血性脑卒中或TIA患者,推荐使用适当剂量的华法林口服抗凝治疗,以预防再发的血栓栓塞事件。华法林的目标剂量是维持INR在2.0-3.0(Ⅰ级推荐,A级证据)。
• 新型口服抗凝剂可作为华法林的替代药物,新型口服抗凝剂包括达比加群、利伐沙班、阿哌沙班以及依度沙班(Ⅰ级推荐,A级证据),选择何种药物应考虑个体化因素。
• 伴有AF的缺血性脑卒中或TIA患者,若不能接受口服抗凝药物治疗,推荐应用阿司匹林单药治疗(Ⅰ级推荐,A级证据)。也可以选择阿司匹林联合氯吡格雷抗血小板治疗(Ⅱ级推荐,B级证据)。
• 伴有AF的缺血性脑卒中或TIA患者,应根据缺血的严重程度和出血转化的风险,选择抗凝时机。建议出现神经功能症状14d内给予抗凝治疗预防脑卒中复发,对于出血风险高的患者,应适当延长抗凝时机(Ⅱ级推荐,B级证据)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#新型口服抗凝药#
37
目前这些优势也无法得到较大体现
101
希望未来能够突破
142
我觉得这种口服药存在很多隐患
123
学习中
116
有意思
105
看看
76
#口服抗凝药#
35
#瓣膜#
35
#房颤患者#
0