Nat Neurosci:痛觉传递存在性别差异
2015-06-30 佚名 生物通
Nature Neuroscience杂志发表的一项最新研究表明,男性和女性之间可能存在根本的痛觉差异。科学家们首次发现,雄性小鼠和雌性小鼠用不同的细胞处理痛觉。这不仅有助于深入理解理解痛觉机制,帮助人们开发更好的药物治疗慢性痛,还会影响人们用小鼠进行基础生物医学研究的方式。慢性痛是当今社会相当普遍的一种健康问题。据统计,世界上约有20-25%的人受到慢性痛的困扰,许多因素都可能引起慢性痛,包括神
Nature Neuroscience杂志发表的一项最新研究表明,男性和女性之间可能存在根本的痛觉差异。
科学家们首次发现,雄性小鼠和雌性小鼠用不同的细胞处理痛觉。这不仅有助于深入理解理解痛觉机制,帮助人们开发更好的药物治疗慢性痛,还会影响人们用小鼠进行基础生物医学研究的方式。
慢性痛是当今社会相当普遍的一种健康问题。据统计,世界上约有20-25%的人受到慢性痛的困扰,许多因素都可能引起慢性痛,包括神经损伤、关节炎、癌症甚至压力。
“之前的研究显示,男性和女性对疼痛的敏感度不同,而且女性更容易患上慢性痛。不过人们一直认为,男性和女性的痛觉处理应该是相同的,”文章的资深作者,McGill 大学的Jeffrey Mogil教授说。“认识到男性和女性的痛觉基础完全不同,这是非常重要的。”
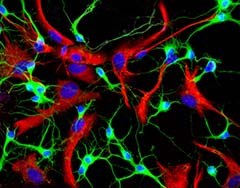
过去的理论是,损伤或炎症位点的痛觉通过小胶质细胞在神经系统中传递。在这项新研究中只有雄性小鼠符合这一理论,干扰小胶质细胞的功能可以有效阻断雄性小鼠的痛觉,但对雌性小鼠却没有影响。
进一步研究表明,在雌性小鼠中传递痛觉信号的是一类完全不同的细胞(T细胞)。不过这一过程的具体机制还有待于进一步研究。
“我们正在开发更复杂更有针对性的下一代镇痛药物,理解痛觉通路的性别差异是非常必要的,”文章的另一位资深作者,多伦多大学的Michael Salter教授说。“我们相信小鼠的神经系统跟人类很相似,尤其是痛觉这样的基础进化功能。这意味着镇痛药物的开发面临着一个重要问题。”
近来,研究雌性动物和细胞越来越受重视。美国NIH不久前公布了新政策,要求临床前研究使用雌性动物和细胞系。
“十五年来科学家们一直认为是小胶质细胞控制着痛觉,但这是基于雄性小鼠研究得出的结论,”Mogil说。“从我们的研究可以看出,要想让所有人从科学研究中获益,实验设计就必须非常仔细。”
原始出处:
Robert E Sorge, Josiane C S Mapplebeck, Sarah Rosen et al.Different immune cells mediate mechanical pain hypersensitivity in male and female mice.Nature Neuroscience, June 29, 2015.doi:10.1038/nn.4053
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Nat#
26
想法很好,期望能早日看见成果
129
看看
122
#ROS#
0
思路很开阔,期待研究结果
99