EMI:风湿性疾病患者活动性肺结核患病率及危险因素的多中心横断面研究
2022-02-01 从医路漫漫 MedSci原创
中国的结核病(TB)病例数量位居世界第三。2010年15岁以上人口活动性肺结核患病率为459/10万。2019年,中国新增结核病患者83.3万人,占全球结核病病例总数的近8.4%。
中国的结核病(TB)病例数量位居世界第三。2010年15岁以上人口活动性肺结核患病率为459/10万。2019年,中国新增结核病患者83.3万人,占全球结核病病例总数的近8.4%。风湿病在中国也是一个严重的问题。据估计,中国大约有2000万风湿病患者。由于原发病和免疫抑制剂的使用,风湿性疾病患者发生ATB的风险很高。结核病和风湿病并存需要考虑许多复杂的问题。结核感染会使风湿病的诊断和治疗变得复杂。另一方面,风湿病患者通常处于免疫功能低下的状态,导致感染持续时间延长,死亡率更高。因此,预防新的结核分枝杆菌(MTB)感染和向ATB的进展对风湿性疾病患者尤为重要。
风湿病患者中存在活动性结核病(ATB)的证据是研究重点,但来自中国的数据报道有限。针对没有服用抗肿瘤坏死因子生物制剂的患者的研究尤其不足。我们的目的是调查这一高危人群中ATB的患病率和危险因素。
我们采用分层多阶段整群抽样策略,以三级医院为基础,进行多中心横断面研究,筛查风湿性疾病患者的ATB。我们评估了风湿性疾病患者中ATB的患病率,并在那些没有服用抗TNF生物制剂的患者中确定了危险因素。
结果显示,按各类风湿病构成比计算的标化患病率为882/100000(95%可信区间为706~1057)。对未服用抗肿瘤坏死因子生物制剂的患者进行多因素Logistic回归分析显示,发生ATB的独立危险因素为系统性红斑狼疮(OR=2.722,95%CI:1.437~5.159,P=0.002)、白塞病(OR=5.261,95%CI:2.07113.365,P<0.001)、近两年服用硫唑嘌呤(OR=2.095,95%CI:0.986~4.450,P<0.05)。在过去两年内接触糖皮质激素≥30 mg/d超过四周(OR=2.031,95%CI:1.247~3.309,p=0.004),且有肺结核病史(OR=6.185,95%CI:3.487~10.969,p<0.001)。
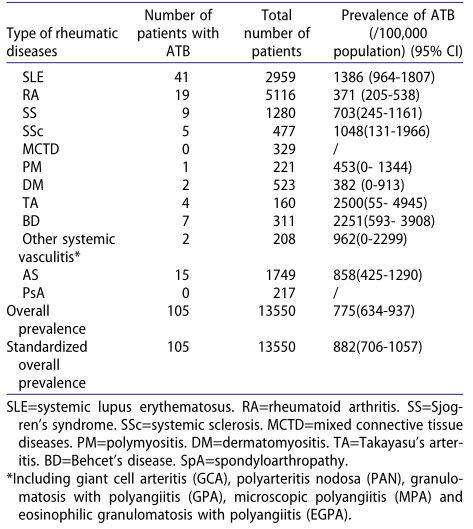
表1 风湿性疾病患者中ATB的患病率。
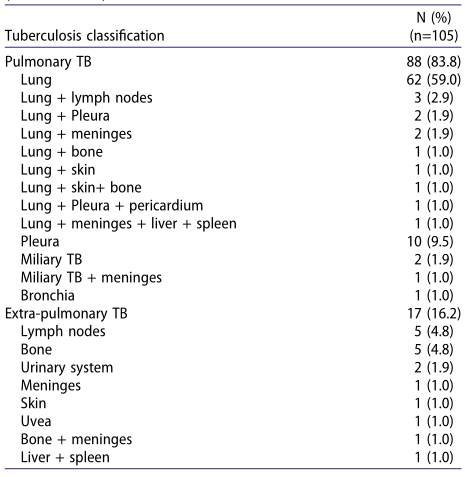
表2 风湿性疾病ATB患者的分类(WS196-2017)。
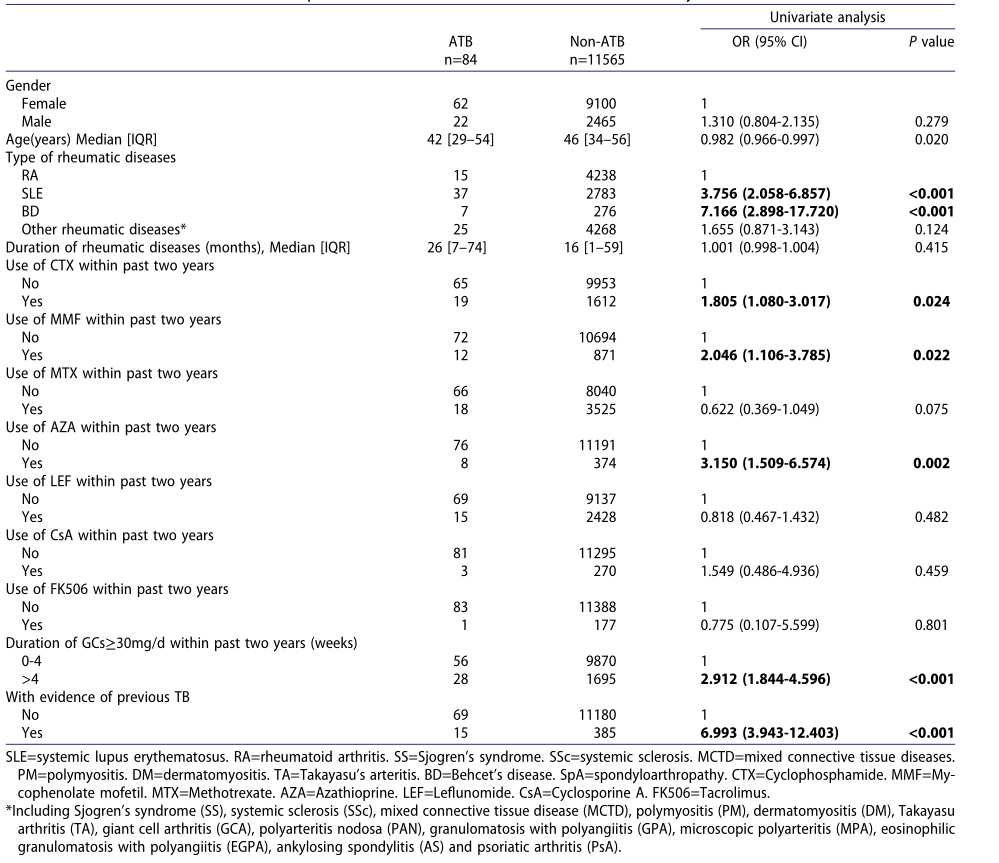
表3 风湿性疾病患者ATB的潜在危险因素的单因素分析

表4 多变量logistic回归分析风湿性疾病患者ATB的潜在危险因素
与普通人群相比,风湿性疾病患者的ATB患病率更高。SLE或BD患者、长期接触中、大剂量糖皮质激素和既往结核病是ATB的独立危险因素。
原文出处: Liu X, Zhang L, Zhang F,et al.Prevalence and Risk Factors of Active Tuberculosis in Patients with Rheumatic Diseases: A Multi-center, Cross-Sectional Study in China.Emerg Microbes Infect 2021 Nov 10
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#活动性肺结核#
78
#活动性#
46
#多中心#
32
#疾病患者#
30
#横断面#
59
#患病率#
34
#结核#
26
#风湿性疾病#
36