European Radiology:深度学习,让冠状动脉CT血管造影实现“双减”!
2022-03-09 shaosai MedSci原创
现阶段,冠状动脉CTA(CCTA)已被确立为疑似阻塞性冠心病(CAD)患者的一线无创成像方式之一。
现阶段,冠状动脉CTA(CCTA)已被确立为疑似阻塞性冠心病(CAD)患者的一线无创成像方式之一。SCOUT-HEART研究的结果表明,与单纯的标准治疗相比,在疑似CAD的标准治疗基础上增加CCTA检查在5年内降低CAD死亡或非致命性心肌梗死(MI)的发生率方面具有优势,这无疑增强了CCTA的应用价值。
尽管CCTA在病变检测方面具有极大优势,但人们对辐射的担忧仍然存在。此外,造影剂引起的肾病(CIN)仍然是这些患者的潜在风险。此外,利用新的先进技术(即CT-FFR)进行CCTA的进一步成像后处理、狭窄评估和准确的功能预测都需要依靠理想的原始图像质量。因此,如何在尽可能低的辐射和造影剂剂量下获得优秀的图像质量引起了巨大的研究兴趣。在CT中使用低电压(在70或80kVp)是实现 "双低(低辐射和对比剂)"剂量目标的最有效方法之一。然而,传统上,低电压的使用仅限于瘦小的病人(BMI<23 kg/m2),并且由于低能量X射线的穿透力降低,会进一步增加图像的噪声。以前的研究报告称,与传统的ASIR-V相比,用深度学习图像重建(DLIR)算法降低CCTA图像噪声的能力更高。然而,DLIR在平衡图像噪声、空间分辨率和图像外观方面的优越性是否在较低的管电压下保持,仍然是未知数。
近日,发表在European Radiology杂志的一项研究评估了70-kvp管电压和高强度设置的DLIR算法(DLIR-H)组合在CCTA检查中的表现,为实现"双低"剂量目标提供了技术支持。
本研究前瞻性地招募了100名进行CCTA检查的患者,并随机分为两组:低剂量组(n = 50),70 kVp,Smart mA的噪音指数(NI)为36HU,对比剂剂量率为16mgI/kg/s,DLIR-H;常规组(n = 50),120 kV,Smart mA的NI为25HU,对比剂剂量率为32mgI/kg/s,60%ASIR-V。比较了两组之间的辐射和对比剂剂量、主观图像质量评分和客观图像质量测量(图像噪声、对比度-噪声比(CNR)和血管的信号-噪声比(SNR))。
与传统组(分别为48.23±6.38 mL和1.65±0.66 mSv)相比,低剂量组使用的造影剂剂量(23.82±3.69 mL,减少50.6%)和辐射剂量(0.75±0.14 mSv,减少54.5%)明显减少(所有P<0.001)。然而,与传统组相比,低剂量组的背景噪音更低(23.57 ± 4.74 HU vs. 35.04 ± 8.41 HU),RCA(48.63 ± 10.76 vs. 29.32 ± 5.52)、LAD(47.33 ± 10.20 vs. 29.27 ± 5.12)和LCX(46.74 ± 9.76 vs. 28.58 ± 5.12)的CNR更高(所有p < 0.001)。
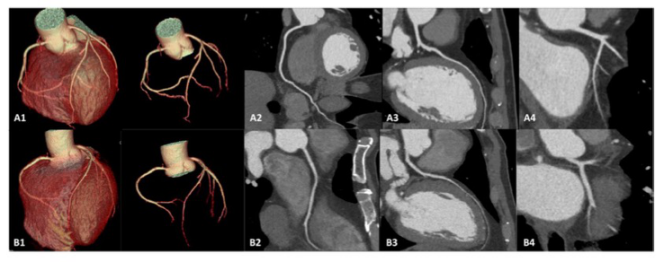
图 低剂量组和常规剂量组的图像质量比较。A1-A4,低剂量组的病例。男性,54岁,BMI为25.61kg/m2,采用70-kvp方案扫描以及高强度深度学习图像重建算法进行重建。图像质量达到主观评分5分,血管边界清晰,图像噪声为12.6 HU;B1-B4,常规剂量组病例。男性,57岁,BMI为25.53 kg/m2,用120-kvp方案扫描以及统计迭代重建算法进行重建。图像质量达到主观评分4分,血管边界有些模糊,图像噪声为17.7H。两位患者均显示冠状动脉正常,但低剂量组的图像质量明显更好。
总之,与传统的120kVp和ASIR-V方案相比,结合70kVp管电压和DLIR-H算法的 "双低 "剂量CCTA方案可在显著降低辐射剂量及造影剂剂量的同时,为正常体型的患者提供更高的图像质量。
原文出处:
Wanjiang Li,Kaiyue Diao,Yuting Wen,et al.High-strength deep learning image reconstruction in coronary CT angiography at 70-kVp tube voltage significantly improves image quality and reduces both radiation and contrast doses.DOI:10.1007/s00330-021-08424-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#冠状动脉CT#
38
#冠状动脉CT血管造影#
40
#PE#
35
#造影#
28