Ann Oncol:中山大学谢芳云发现鼻咽癌行新辅助化疗在生存率方面优于辅助化疗
2013-04-26 Ann Oncol dxy
在2013年4月23日在线出版的《肿瘤学年鉴》(Annals of Oncology)杂志上,发表了我国中山大学谢芳云教授等人的一项最新研究结果,该研究通过随机、对照试验(RCT),利用荟萃分析方法,对新辅助化疗(NACT)及辅助化疗(AC)在鼻咽癌(NPC)患者治疗中的疗效进行了论证。 该研究对电子数据库及稿件进行了全面搜索,以从符合条件的研究中获取适用于荟萃分析的相关RCT数据。研究人员通过
在2013年4月23日在线出版的《肿瘤学年鉴》(Annals of Oncology)杂志上,发表了我国中山大学谢芳云教授等人的一项最新研究结果,该研究通过随机、对照试验(RCT),利用荟萃分析方法,对新辅助化疗(NACT)及辅助化疗(AC)在鼻咽癌(NPC)患者治疗中的疗效进行了论证。
该研究对电子数据库及稿件进行了全面搜索,以从符合条件的研究中获取适用于荟萃分析的相关RCT数据。研究人员通过随机及/或固定效应模型,对同时总生存率(OS)和风险比(HR)、局部复发率(LRR)、远端转移率(DMR)及相对风险(RR)等参数进行了关注。同时还进行了亚组分析及敏感度分析。
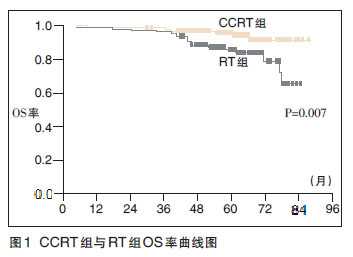
在NACT组中,共有6项试验符合条件(n = 1418),AC组则有5项(n = 1187)。研究结果显示,NACT组死亡HR为0.82 [95%置信区间(CI) 0.69-0.98, P = 0.03],这与5.13%的3年后绝对生存获益相对应。研究人员同时发现,NACT组中的DMR出现显著降低(P = 0.0002; RR 0.69, 95% CI 0.56-0.84)。但该研究未发现LRR降低(P = 0.49; RR 0.90, 95% CI 0.66-1.22)。额外接受AC治疗患者的LRR较低(P = 0.03; RR 0.71, 95% CI 0.53-0.96)。但研究未发现AC组患者取得OS及DMR获益。
谢教授等人最终认为,NACT可有效改善NPC患者OS并可降低DMR,但不能降低患者LRR。而AC仅有助于改善NPC患者的局部复发情况。
与鼻咽癌相关的拓展阅读:
- Cancer Res.:鼻咽癌细胞系中发现干细胞样细胞亚群新特征
- Cancer Res:鼻咽癌放疗后复发及治疗耐受的重要原因
- Lancet Oncol:III期临床研究证实晚期鼻咽癌标准治疗方案未使患者获益
- Radiother Oncol:调强放疗对鼻咽癌患者临床疗效较好
- JNCI:吸烟影响鼻咽癌发病及诱导EB病毒活动
- 中山大学肿瘤防治中心鼻咽癌诊治技术获重要进展 更多信息请点击:有关鼻咽癌更多资讯

Significant efficacies of neoadjuvant and adjuvant chemotherapy for nasopharyngeal carcinoma by meta-analysis of published literature-based randomized, controlled trials
Background
We carried out this meta-analysis to demonstrate efficacies of neoadjuvant chemotherapy (NACT) and adjuvant chemotherapy (AC) for nasopharyngeal carcinoma (NPC) patients based on randomized, controlled trials (RCTs).
Patients and methods
We comprehensively searched electronic databases and manuscripts for RCTs and extracted data from eligible studies for meta-analysis. Overall survival (OS) with hazard ratios (HRs), locoregional recurrence rate (LRR) and distant metastasis rate (DMR) with relative risks (RRs) were concerned using random and/or fixed-effects models. Subgroup and sensitivity analyses were also carried out.
Results
Six trials in NACT group (n = 1418) and five in AC group (n = 1187) were eligible. HR of death for NACT was 0.82 [95% confidence interval (CI) 0.69–0.98, P = 0.03], corresponding to an absolute survival gain of 5.13% after 3 years. Significant reduction of DMR (P = 0.0002; RR 0.69, 95% CI 0.56–0.84) was also found from NACT. But no decrease in LRR (P = 0.49; RR 0.90, 95% CI 0.66–1.22) was observed. Patients receiving additional AC had lower LRR (P = 0.03; RR 0.71, 95% CI 0.53–0.96). But no benefit of OS and DMR were seen in AC.
Conclusions
NACT can effectively enhance OS and reduce DMR, not LRR in NPC. And AC only helps to better control locoregional recurrence of NPC.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
26
#新辅助#
33
#生存率#
36
#中山大学#
34