Nat Methods:新技术可实现对机体5D成像 或助力疾病诊断和治疗
2017-01-16 生物谷 生物谷
图片来源:www.phys.org 近日,一项刊登在国际杂志Nature Methods上的研究报告中,来自英国剑桥大学等处的研究人员通过研究开发了一种新型的成像分析技术,该技术能够帮助寻找重要的生物学分子(疾病迹象),同时还能够帮助快速分析研究这些分子之间如何相互作用,这种名为超光谱矢量分析(Hyper Spectral Phasor analysis,HySP)的技术或能利用手机

图片来源:www.phys.org
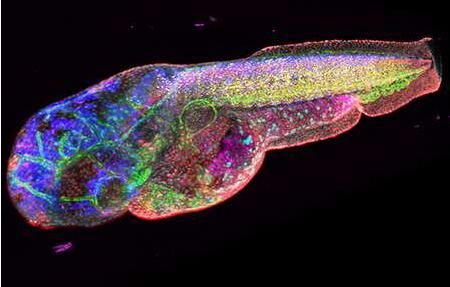
近日,一项刊登在国际杂志Nature Methods上的研究报告中,来自英国剑桥大学等处的研究人员通过研究开发了一种新型的成像分析技术,该技术能够帮助寻找重要的生物学分子(疾病迹象),同时还能够帮助快速分析研究这些分子之间如何相互作用,这种名为超光谱矢量分析(Hyper Spectral Phasor analysis,HySP)的技术或能利用手机图片来帮助诊断和监测疾病。
文章中,研究者利用荧光成像技术来锁定细胞和组织中的蛋白和其它分子,荧光成像能够帮助研究人员理解癌症或其它疾病中大量产生的分子,而且相关信息还能用于对疾病进行诊断或寻找治疗性药物所作用的靶点。观察组织样本或细胞中的一两种分子非常简单,但这并不能够清楚地阐明真实情况下这些分子的作用以及行为机制,因此科学家们就需要进行深入研究来寻找更多特殊分子。
研究者Francesco Cutrale说道,通过观察多个靶点,或者随着时间延续追踪靶点,我们就能够更好地观察并且分析复杂有机体中发生的事件;当前研究人员必须分开观察不同的标记,随后再应用复杂的技术将不同标记叠加在一起来阐明这些标记分子之间的关联,本文中研究者开发的新技术HySP就能够在一个循环中对多个不同分子进行分析研究。
想象一下研究者看到了18个靶点,利用这种技术就可以对这些靶点进行一次性快速研究,此外,HySP技术还能够有效过滤对真正信号的干扰情况,甚至是在信号极其微弱的情况下依然能够有效发挥作用。Fraser说道,该技术使用的计算时间较少,而且我们也并不需要使用昂贵的成像仪器。在实验室模型中,研究人员能够利用基因操作来标记分子,但这在人类机体中根本行不通,在人类机体研究中,研究人员不得不利用分子的内在信号来进行研究。
这些内在信号,也就是来自生物分子的天然荧光,其能够通过成像来进行观察,然而利用计算机算法就能够在复杂背景下有效寻找信号微弱的分子,这样就能够靶向作用机体中的特殊靶点。研究人员希望在未来几年中能够对本文中所开发的新技术进行检测来帮助治疗肺部损伤的士兵们进行治疗,而且未来对于临床医生们而言也有望利用HySP技术来对皮肤损伤的手机图片进行分析来确定患者是否具有癌变风险。
研究者认为,他们能够确定随着时间变化这些损伤是否会改变颜色或形状,随后临床医生们就会对患者进行检查来进一步确定病情。当前科学家和临床医生们都希望能够快速高效地工作,而本文中这种新技术就给这些研究者们带来了巨大帮助。
原始出处
Francesco Cutrale, Vikas Trivedi, Le A Trinh, Chi-Li Chiu, John M Choi, Marcela S Artiga & Scott E Fraser.Hyperspectral phasor analysis enables multiplexed 5D in vivo imaging.Nat Methods.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Nat#
17
#疾病诊断#
21
#MET#
21
学习了,谢谢作者分享!
42
#新技术#
18