J Gastroenterology: 克罗恩病患者中肠源干细胞的修饰与疾病活动存在相互影响
2018-09-08 MedSci MedSci原创
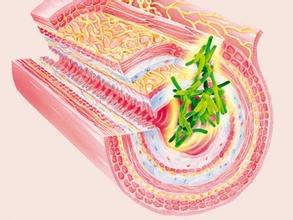
肠干细胞(ISCs)在维持体内平衡以及受损肠上皮的再生中发挥着不可或缺的作用。然而,克罗恩病(CD)的炎症环境是否会影响常驻小肠干细胞的特性仍然不明确,本项研究通过体外实验阐明了他们之间的关系。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#GAS#
29
#AST#
42
#Gastroenterol#
36
#疾病活动#
38
#Gastroenterology#
28
#修饰#
35
学习了谢谢
65