European Radiology:DCE-MRI可实现肝纤维化评估的“一步到位”!
2021-12-28 shaosai MedSci原创
为了无创地进行组织灌注测量,人们使用了各种灌注成像技术,其中动态对比增强磁共振成像(DCE-MRI)是最常用的技术之一。
 为了无创地进行组织灌注测量,人们使用了各种灌注成像技术,其中动态对比增强磁共振成像(DCE-MRI)是最常用的技术之一。然而,DCE-MRI在评估肝脏实质和肝脏肿瘤方面的应用很有限。这是由于DCE-MRI需要较高的时间分辨率来追踪组织信号强度和血管增强峰值的动态变化。为了达到高时间分辨率,空间分辨率和图像质量往往会受到影响。此外,在肝脏成像中,数据经常受到运动伪影的影响。因此,DCE-MRI往往不能为临床提供满足诊断的图像质量。
为了无创地进行组织灌注测量,人们使用了各种灌注成像技术,其中动态对比增强磁共振成像(DCE-MRI)是最常用的技术之一。然而,DCE-MRI在评估肝脏实质和肝脏肿瘤方面的应用很有限。这是由于DCE-MRI需要较高的时间分辨率来追踪组织信号强度和血管增强峰值的动态变化。为了达到高时间分辨率,空间分辨率和图像质量往往会受到影响。此外,在肝脏成像中,数据经常受到运动伪影的影响。因此,DCE-MRI往往不能为临床提供满足诊断的图像质量。
GRASP MRI是一种结合了平行成像、径向采集和压缩感知的技术。该技术通过同时使用压缩传感和平行成像来加快扫描时间,并且由于其采用径向采集扫描,因此对运动的敏感性较低。
近日,发表在European Radiology杂志的一项研究应用GRASP DCE-MRI同时评估肝纤维化患者的肝脏灌注和形态,为该类患者的准确诊断及评估提供了技术支持及参考依据。
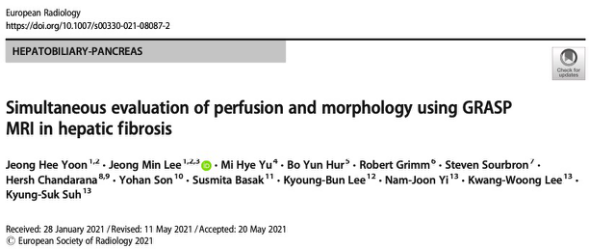
本研究预定进行肝脏活检或切除的参与者被纳入其中(NCT02480972)。图像以12秒的时间分辨率重建用于形态学评估,以3.3秒的时间分辨率重建用于定量评估。形态学图像的质量按四分法评估,并记录肝脏成像报告和数据系统的评分分级。对不同纤维化阶段的DCE-MRI定量参数和具有不同LR特征的肝细胞癌(HCC)进行了比较。
对64名参与者(男性=48)的DCE-MRI进行了分析。在整个检查过程中,整体图像质量始终保持在3.5±0.4至3.7±0.4。与F0-F1的参与者相比,F2-F3(n = 18, 175 ± 110 mL/100 mL/min)和F4(n = 12, 98 ± 47 mL/100 mL/min)的门静脉血流明显减少(n = 34, 283 ± 178 mL/100 mL/min,所有P < 0.05)。在F4的参与者中,动脉分数和细胞外体积明显高于F0-F1和F2-F3的参与者(P < 0.05)。与表现非LR-M特征的HCC(n = 16)相比,具有LR-M的HCC(n = 5)的MTT明显延长,动脉血流量较低(p < 0.05)。
图 66岁男性的自由呼吸T1-加权图像。平扫(a)、动脉(b)、门静脉(c)和延迟相(d)是在不屏气的情况下获得的。时间分辨率为12秒。在任何阶段都没有观察到明显的运动伪影。
本研究表明,DCE-MRI可以从单一的采集数据集中同时获得形态学成像信息,且不同纤维化阶段的门静脉血流有明显的差异,这为肝纤维化患者的风险分层及评估提供了参考依据。
原文出处:
Jeong Hee Yoon,Jeong Min Lee,Mi Hye Yu,et al.Simultaneous evaluation of perfusion and morphology using GRASP MRI in hepatic fibrosis.DOI:10.1007/s00330-021-08087-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#DCE-MRI#
51
#PE#
43
#肝纤维#
52
学习学习学习学习学习学习学习学习学习学习学习我学习学习学习
64
学习了
52