NEJM:抑制心脏骤停后节律性和周期性EEG活动对患者神经功能预后的影响
2022-03-01 MedSci原创 MedSci原创
对于心脏骤停昏迷后出现节律性和周期性EEG活动的患者,抗癫痫方案不能降低3个月时神经功能不良预后风险。

据报道,10-35%的心脏骤停昏迷患者会出现与癫痫发作相关的节律性和周期性脑电图(EEG)活动,导致患者神经系统预后较差。近日研究人员考察了在出现节律性和周期性脑电图患者中进行抗癫痫药物治疗对神经系统预后的影响。

研究人员开展了一项开放标签试验,因心脏骤停昏迷的幸存者在连续脑电图监测中检测到节律性和周期性脑电图后参与研究,在标准治疗基础上,随机接受抗癫痫药物治疗,抑制节律性和周期性脑电图活动至少48小时或对照。研究的主要结果是3个月时脑功能分级量表(CPC)得分,分为预后良好(CPC评分表示无、轻度或中度残疾)或不良预后(CPC评分表示严重残疾、昏迷或死亡)。次要结果是死亡率、重症监护病房(ICU)住院时间和机械通气的持续时间。
172例患者参与研究,其中88人接受抗癫痫治疗,84人接受对照。患者心脏骤停后平均35小时检测到节律性或周期性EEG,其中有98例(62%)出现肌阵挛。抗癫痫治疗组88例患者中有49例(56%)实现连续48小时节律性和周期性EEG活动完全抑制,对照组83例患者中有2例(2%)。3个月时,抗癫痫治疗组88名患者预后不佳(90%),对照组84名患者中有77名(92%,差异2%)。3个月时,抗癫痫治疗组患者的死亡率为80%,对照组为82%。抗癫痫治疗组在ICU平均住院时间和机械通气的平均持续时间略长于对照组。
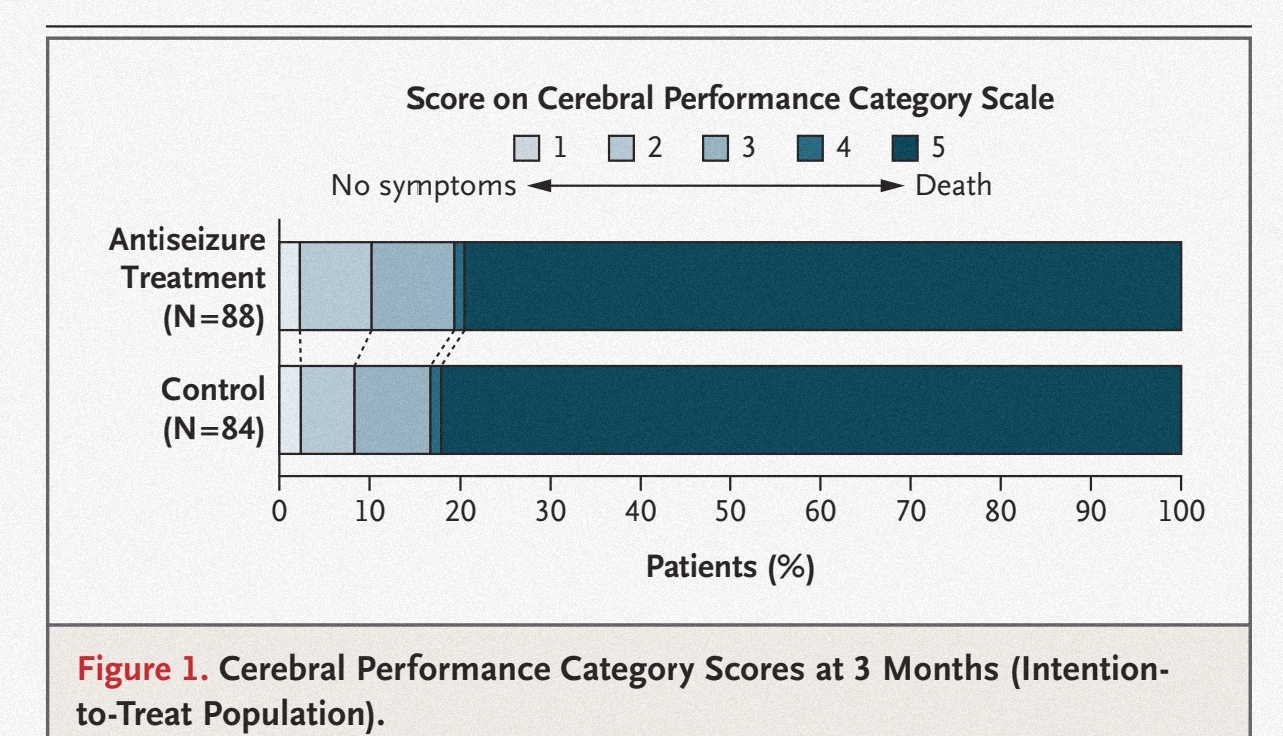
组间神经功能预后差异
研究发现,对于心脏骤停昏迷后出现节律性和周期性EEG活动的患者,抗癫痫方案不能降低3个月时神经功能不良预后风险。
原始出处:
Barry J. Ruijter et al. Treating Rhythmic and Periodic EEG Patterns in Comatose Survivors of Cardiac Arrest. N Engl J Med,February 24, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#EEG#
44
#节律性#
40
#神经功能#
43
#功能预后#
32
学习一下
50
学习
0
学习了
49