JACC:卒中后卵圆孔未闭封堵术,可减少卒中复发
2016-02-23 崔倩 译 MedSci原创
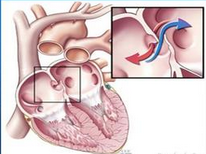
对于卵圆孔未闭(PFO)封堵加药物治疗 vs 单纯药物治疗隐源性脑卒中的效果是不确定的。研究人员进行了第一次汇总分析,该分析包括了已完成的随机试验中比较隐源性脑卒中患者进行PFO封堵 vs 药物治疗的个体参与者的数据。该分析包括对2个设备(STARFlex[伞式封堵器] [NMT Medical公司,马萨诸塞州波士顿市]和Amplatzer PFO封堵器[盘封堵器] [AGA医疗/圣犹达医疗用品,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#卒中后#
25
#封堵术#
38
#JACC#
40
#ACC#
24
#卒中复发#
32