JAMA Netw Open:年轻结直肠癌患者生存率反而更低,这是什么道理?
2021-06-17 MedSci原创 MedSci原创
早发性结直肠癌(CRC)的生存率与老年人结直肠癌的生存率相比如何?
在美国50岁以下的成年人中,结直肠癌(CRC)是第二大最常见的癌症和第三大癌症死亡原因。虽然对早期结直肠癌没有明确的定义,但在已发表的文献中,年龄小于50岁似乎是一个普遍的标准。使用这一标准的部分原因是,在过去20年中美国独立专家小组发表了一些建议,对平均风险水平为50岁的人进行CRC筛查。
早发CRC(即在50岁诊断的CRC)具有独特的临床、遗传和表观遗传特征,因此,在年龄超过50岁的个体中,它可能与诊断的结肠癌不同的生存率有关。关于早期结直肠癌患者生存期与老年结直肠癌患者生存期的比较报道并不一致。
此外,早期结直肠癌患者更有可能在晚期被诊断。考虑到小于50岁的年龄范围很广,不同年龄的早期结直肠癌生存率可能存在异质性。因此,有研究小组使用国家癌症数据库(NCDB)进行分析以验证这些假设,该研究结果近日发表在JAMA Netw Open杂志上。
这项队列研究纳入的患者年龄为0-90岁,于2004年1月1日至2015年12月31日诊断为原发性结直肠癌。本研究选取51 ~ 55岁确诊的患者作为参照组,并定义为晚发性结直肠癌。排除年龄在50岁的患者,尽量减少该年龄人群中明显的筛查检测偏倚,考虑到这些患者的早期表现不成比例。所有的统计分析时间为2020年1月4日至2020年12月26日。采用Kaplan-Meier分析和Cox比例风险回归评估总生存率。
研究结果显示,在769871例结直肠癌患者中(377890例(49.1%)为女性;636791名白人(82.7%),353989名(46.0%)死亡,102168名(13.3%)诊断为早发性大肠癌,78812名(10.2%)诊断为晚发性大肠癌。在未经校正的分析中,与年龄在51岁到55岁之间的患者相比,早发性大肠癌患者的10年生存率较低。
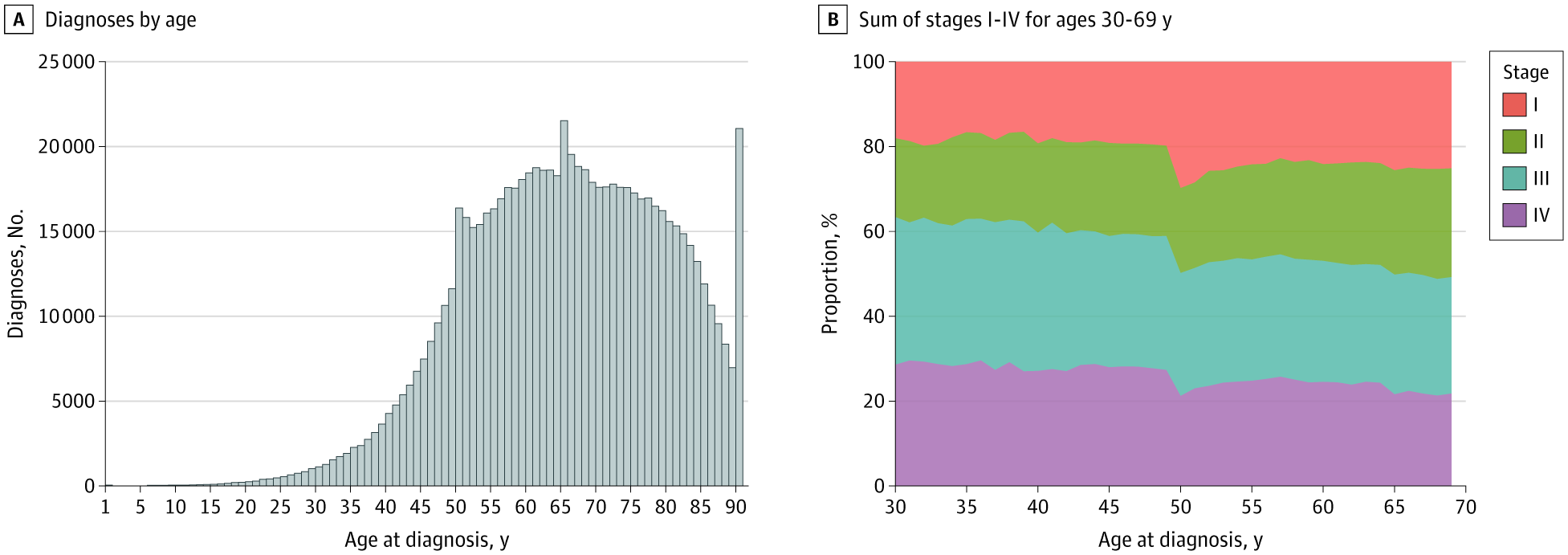
国家癌症数据库中结直肠癌患者诊断和分期的年龄分布
然而,在调整了与死亡率相关的其他因素(最显著的是分期)后,与51岁至55岁的患者相比,早发性大肠癌患者的死亡风险较低。在校正分期的模型中,早发大肠癌患者的HR为0.89。在35岁到39岁以及I期和II期诊断的个体中,存活优势最大,而在25岁或更小以及III期到IV期诊断的个体中,存活优势不存在。

早期和晚期结直肠癌的总死亡率比较
这项研究发现,在未经调整的分析中,较年轻的CRC患者死亡率增加,这与在疾病的后期阶段被诊断有关。这也表明,如果对较年轻的患者进行更多的筛查使得他们的疾病能够在早期阶段被发现,可能会降低他们的死亡率。
在年轻个体中与早发CRC相关的生存优势应该谨慎解释,因为这种优势规模较小,并且随着年龄和阶段的不同而存在异质性。需要进一步的研究来了解早期结直肠癌患者中不同年龄和分期生存的潜在异质性。
参考文献:Cheng E, Blackburn HN, Ng K, et al. Analysis of Survival Among Adults With Early-Onset Colorectal Cancer in the National Cancer Database. JAMA Netw Open. 2021;4(6):e2112539. doi:10.1001/jamanetworkopen.2021.12539
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#NET#
32
#患者生存#
46
#PE#
28
#生存率#
33
#结直肠#
32
学习了
51
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
54
学习了
56
#学习#学习了
61
加强中老年人筛查
61