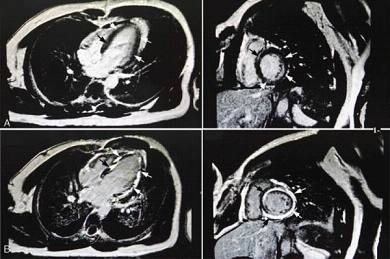
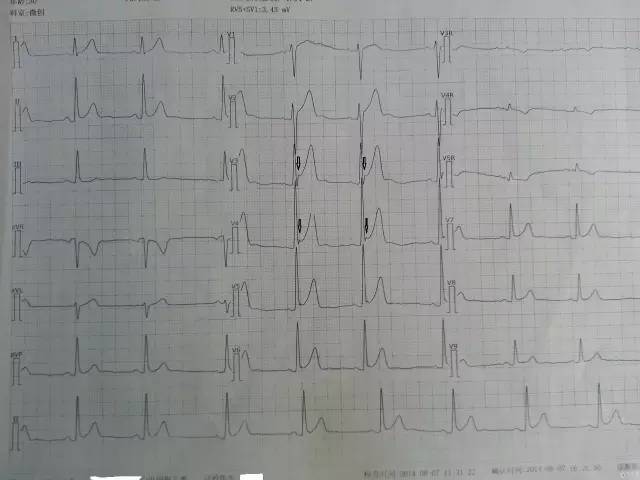
Medicine:阜外医院杨艳敏等总结ST段抬高心肌炎的患者特征:核磁可见斑片状延迟强化,及时诊治者预后良好
2017-07-10 文韬 中国循环杂志
临床上常见一类病人,就是心电图ST段抬高,但冠状动脉造影正常,有些患者最终诊断为心肌炎。这类病人可称为类似ST段抬高急性心肌梗死样的心肌炎。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#DIC#
35
#CIN#
43
#阜外医#
44
#阜外医院#
47
#ST段抬高#
32
#Medicine#
22
#Med#
28
#患者特征#
28
#ST段#
0
好!
60