Eur Raidol:肝癌侵犯胆管后,栓塞化疗术前是否需要进行胆管引流?
2017-12-14 shaosai MedSci原创
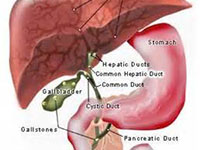
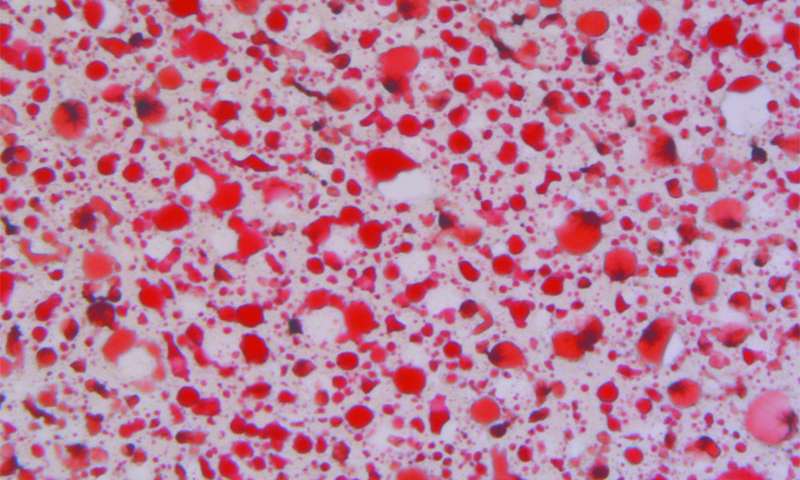
本研究旨在验证肝癌(HCC)侵犯胆管后,栓塞化疗术前进行胆管引流的必要性,并将结果发表在Eur Raidol上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#IDO#
28
#AID#
36
要判断是否达到引流条件.评估患者身体状况.不可一概而论
74
学习一下谢谢分享
79
学习一下谢谢分享
58
学习一下谢谢分享
63
学习
83
肝癌侵犯胆管.
28
学习了.谢谢分享!
21
#胆管#
27