Diabetes Technol Ther:挑战指南!并不是所有的高分化型甲状腺癌儿童患者均要接受全甲状腺切除
2016-11-29 MedSci MedSci原创
目前的指南建议高分化型甲状腺癌(WDTC)儿童患者应行甲状腺全切除术。然而,这些指南是在现有高分辨率成像技术之前所制定的。本研究推测应有部分儿童患者或可经腺叶切除术而得到完全治愈。采用回顾性分析设计,纳入2004年至2015年接受治疗的73名WDTC儿童患者。我们采用了两种不同的风险分层标准。首先研究人员确定符合ATA“低风险”标准的患者数量,定义为疾病分期为N0 / NX或偶然的N1a。然后,研
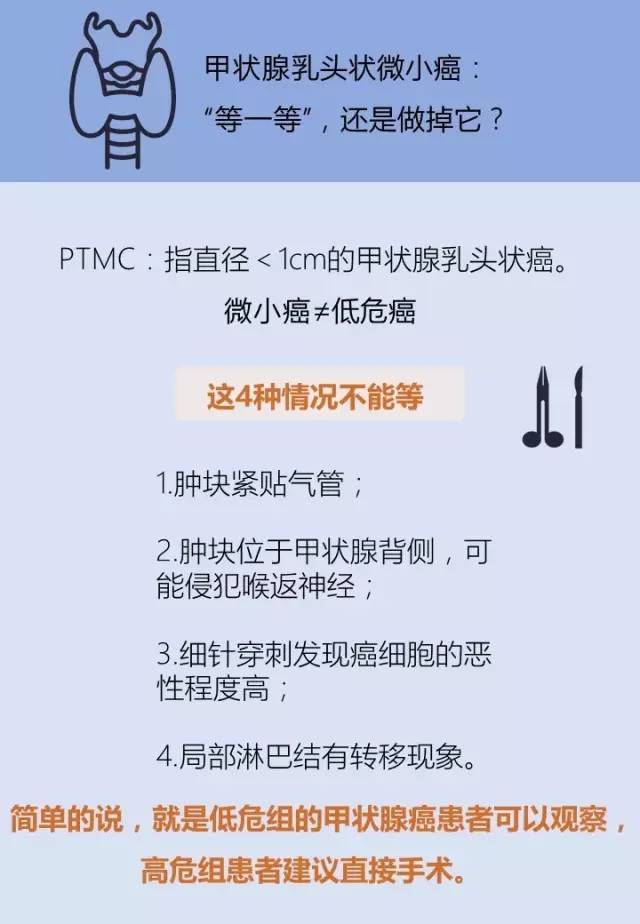
目前的指南建议高分化型甲状腺癌(WDTC)儿童患者应行甲状腺全切除术。然而,这些指南是在现有高分辨率成像技术之前所制定的。本研究推测应有部分儿童患者或可经腺叶切除术而得到完全治愈。
采用回顾性分析设计,纳入2004年至2015年接受治疗的73名WDTC儿童患者。
我们采用了两种不同的风险分层标准。首先研究人员确定符合ATA“低风险”标准的患者数量,定义为疾病分期为N0 / NX或偶然的N1a。然后,研究人员确定了一套“低风险”的组织病理学标准,包括单发肿瘤≤4cm,没有预定义的高危因素,确定符合这些标准的患者的比例。
最终研究纳入27名(37%)男性和46名(63%)女性,平均年龄为13.4岁。同侧和对侧多灶性病灶分别有27名(37%)和19名(26%)患者。37名(51%)的患者有淋巴结转移(N1a=18/N1b=19)。术前超声确定了所有存在淋巴结疾病的患者。73名患者中,39名(53.4%)患者符合ATA 低风险标准,16名(21.9%)符合非常低风险的标准。所有的非常低风险的患者在初步治疗后均表现出良好的反应,在平均随访36.4个月后,无持久性/复发。
总而言之,超声和组织病理学确定了可能受益于叶切除术的患者人群,从而避免了与全甲状腺切除术相关的风险,以及潜在的医疗和社会心理问题的发生。研究人员构建了一个临床框架,以刺激讨论将叶切除术作为低风险患者治疗的一个选择。
原始出处:
Polonsky WH, et al. Is it time to reconsider lobectomy in low-risk paediatric thyroid cancer? Diabetes Technol Ther. 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BET#
30
#Diabetes#
22
#DIA#
31
#高分化#
37
#TEC#
29
#分化型甲状腺癌#
24
了解一下
64
这个可以
45
儿童甲状腺癌
44
非常精彩!
51