
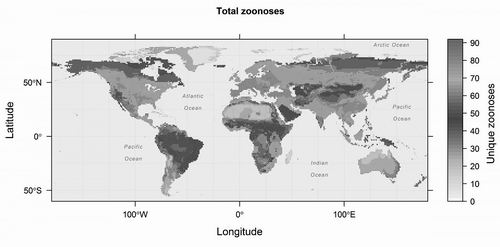
研究人员绘制的动物传染病地图 图片来源:DREW KRAMER
目前,大多数人类流行传染病来源于哺乳动物。但人们仍对哺乳动物—人病原体传播途径的全球模式知之甚少。来自美国卡里生态系统研究所和佐治亚大学的研究人员集合了记录哺乳动物—人疾病的世界地图,旨在分析能否预测新动物传染病的出现。相关成果近日刊登于《寄生虫学趋势》。
这些地图包括狂犬蝙蝠、携带中东呼吸综合征病毒的骆驼以及超过2000种啮齿类动物等陆生哺乳动物数据。一般而言,源于非人类宿主(人畜共患病)病原体引发的疾病的暴发被认为是不可预测的,但这些地图揭示了若干已被研究的模型。
“令我感到惊讶的是,生物传染病的热点地区与生物多样性热点并不匹配。”该研究报告第一作者、卡里生态系统研究所的Barbara Han说,“例如,热带地区具有很高的物种多样性,因此我们希望看到更多动物传染病寄生虫和病原体在热带地区也具有相似的模式。我们虽然在热带地区发现更多的动物传染病宿主,但却在温带地区发现更多动物传染病。原因可能是这些疾病能发生在多重宿主中。”
该地图揭示,超过10%的啮齿类动物是动物传染病宿主,携带了85种不同的疾病。尽管该研究涵盖的灵长类动物不多,但有21%是宿主。研究人员还指出,尽管蝙蝠“臭名昭著”,但其携带的疾病(25种)少于啮齿类动物(85种)、灵长类动物(61种)和食肉动物(83种)。另外,欧洲和俄罗斯是啮齿类宿主的全球热点地区,中南美洲是蝙蝠热点地区,而灵长类宿主主要集中在赤道非洲。而且,与其他病原体类型相比,哺乳动物携带更多的细菌。
“了解动物分布在哪里以及原因是什么似乎与人们的日常生活无关。”Han说,“但较大规模的突破恰好依靠这类基础科学知识。”
原始出处:
Han BA, Kramer AM, Drake JM. Global Patterns of Zoonotic Disease in Mammals. Trends Parasitol. 2016 Jul;32(7):565-77.
Han BA, Schmidt JP, Alexander LW, Bowden SE, Hayman DT, Drake JM. Undiscovered Bat Hosts of Filoviruses. PLoS Negl Trop Dis. 2016 Jul 14;10(7):e0004815
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ENDS#
37
#RASI#
30
#SIT#
22
#trend#
21
#ASIT#
26