【一般资料】
患者男,65岁,
【主诉】
因反复发热就诊后影像学检查发现左肾占位收住入院
【现病史】
患者无腰腹部疼痛,无尿频、尿急、尿痛及肉眼血尿,大小便基本正常。
【体格检查】
入院体温:37.2℃,血压:113/73mmHg,查体双肾区无明显红肿及隆起,肾脏无叩击痛,双肾区未闻及血管杂音,沿双侧输尿管行程区无压痛。
【辅助检查】
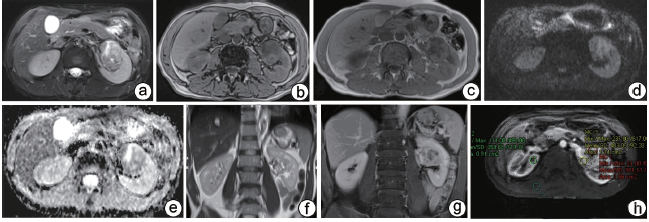
生化指标:尿常规:上皮细胞7.40个/μl,余无特殊;血常规及生化:白细胞计数9.78×109/L,粒细胞计数7.22×109/L,单核细胞计数0.80×109/L;白球比值1.21,白蛋白(溴甲酚绿法)33.4g/L,总蛋白(双缩脲法)60.9g/L,谷草转氨酶(IFCC法)11.4U/L。MRI扫描示左肾轮廓失常,左肾上极见一团块状异常信号影,边界尚清,形态欠规则,大小约3.8cm×3.9cm×2.7cm,其内信号欠均匀,与正常肾实质信号相比,T2WI病灶主体呈稍低信号,其内见斑片状高信号,T1WI呈病灶主体呈稍低信号,其内见斑片状稍高信号,DWI呈稍高信号,正反相位未见明显信号减低,增强扫描病灶可见明显不均匀强化,延迟期可见造影剂退出,病灶区动态增强曲线部分呈速升速降型、部分呈速升平台型,病灶累及中上组肾盏及肾盂,腹膜后未见明显肿大淋巴结(图a~i)。
【治疗】
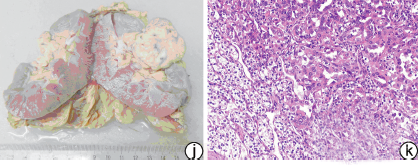
手术及病理:行腹腔镜左肾根治性切除术,所见左侧肾脏大小9.2cm×5.5cm×4.0cm,切开于肾盂处见一灰黄色结节,结节大小3.5cm×3.3cm×3.0cm,似有包膜,结节切面呈灰黄灰褐色,局部区域伴出血、胶冻样,质地中等,与周围组织界限清,其余切面灰黄灰褐色,质地中等,皮质厚0.5cm,髓质厚0.8~1.5cm,皮髓质界限清。病理初步诊断肾盂肾透明细胞癌(FuhrmanⅣ级),免疫组化显示抗体CD10++++,RCC+++,Vimentin+++,CKpan+++,Ki-671-5%局灶区域30%,阴性抗体类型:CD117、TFE-3/P53、CK5/6,免疫组化结果支持肾盂透明细胞癌(FuhrmanⅣ级)(图j~k)。

【讨论】
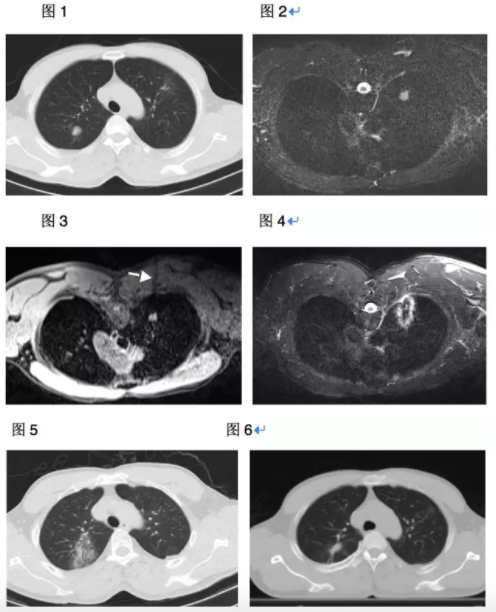
主要特点肾盂的原发性肿瘤比较少见,多为高级别尿路上皮癌,而由于组织细胞发生变异化生,肾盂尿路上皮癌可有多种特殊的组织学表现,主要包括:肉瘤样癌、鳞癌、微乳头癌及透明细胞癌等,国外有关肾盂透明细胞癌的报道非常少见,国内目前就肾盂透明细胞癌的报道只有2例,其病理表现部分癌细胞类似肾透明细胞癌,病灶位于肾窦区内,临床常有血尿症状,尿路造影可见肾盂肾盏内不规则的固定充盈缺损影,肾盂肾盏扩大变形,病灶常呈浸润性性生长,与正常肾实质及输尿管分界不清,增强扫描低到中等强化。部分肿瘤组织发生缺血坏死、囊变、出血,CT表现为混杂密度影,MRI表现T1WI呈混杂低信号,T2WI呈混杂高信号,增强扫描皮质期轻中度强化,合并囊变、坏死时强化不明显。其病理表现部分癌细胞类似肾透明细胞癌,胞质丰富,淡染或空泡状,核位于中央,胞界清楚,呈巢或片状,与尿路上皮癌有过渡,弥漫浸润肾实质。分化差的肾盂尿路上皮癌伴有广泛的透明细胞特征时需与肾透明细胞癌鉴别,仔细寻找尿路上皮癌成分,并行免疫组化标记有助于准确诊断。2.2鉴别诊断①肾透明细胞癌:肾脏最常见恶性肿瘤,早期常无症状,瘤体增大时临床主要表现为血尿、肾区痛、肿块三大症状。瘤体血供丰富,多伴出血囊变,少数可有钙化,CT表现肾轮廓改变,病灶密度不均匀,增强扫描皮质期明显不均匀强化,强化程度近似肾皮质,而后明显廓清,假包膜延迟强化,向肾外侵犯显示肾周筋膜毛玻璃样密度增高、消失、增厚。MRI上肿块多为混杂信号,周围有低信号的假包膜带,增强各期与CT表现相同;有研究表明尿路上皮癌来源的透明细胞CK7和CK20呈阳性,肾细胞抗原阴性,而肾透明细胞癌CK7和CK20呈阴性,肾细胞抗原阳性。②肾集合管癌:肾轮廓多完整,常同时累及皮质和肾盂,病灶形态不规则,无假包膜,边缘不清,呈侵袭性生长,易伴出血、坏死、囊变,且不均匀轻度强化,增强扫描皮质期无明显强化,之后轻度渐进性晚期强化。总之,由于肾盂尿路上皮癌的特殊类型(如:透明细胞癌等)非常少见,其影像学诊断还需要不断积累经验,并结合病理提高诊断的准确性。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞癌#
26
#透明细胞癌#
28
学习
91
谢谢分享学习一下
88