多学科诊断(MDT)后腹膜软组织肉瘤1例
2013-07-27 复旦大学附属中山医院腹部软组织肉瘤MDT协作组 陆维祺 周宇 中国医学论坛报
病历简介 患者女性,57岁,2010年9月起出现左下肢肿胀、酸痛。门诊体检在腹部脐左下方触及巨大包块,质硬无压痛。腹部CT检查发现左下腹占位伴左肾盂扩张积水。考虑可能为后腹膜间叶源性肿瘤收入院。 入院检查 超声检查显示腹腔实质性低回声团块,来源于腹膜后,左输尿管上段扩张伴左肾盂积水,右肾、右输尿管未见异常。 CT血管造影(CTA)示
病历简介
患者女性,57岁,2010年9月起出现左下肢肿胀、酸痛。门诊体检在腹部脐左下方触及巨大包块,质硬无压痛。腹部CT检查发现左下腹占位伴左肾盂扩张积水。考虑可能为后腹膜间叶源性肿瘤收入院。
入院检查
超声检查显示腹腔实质性低回声团块,来源于腹膜后,左输尿管上段扩张伴左肾盂积水,右肾、右输尿管未见异常。
CT血管造影(CTA)示左侧腹膜后巨大肿块包绕腹主动脉下段及左侧髂血管,肠系膜下动脉、腹主动脉受压改变(图1、2)。CT尿路造影(CTU)显示左侧输尿管受侵,腹膜后多发肿大淋巴结。胸部CT检查未见异常。

图1 化疗前CT动脉期显像,肿块大小
126 mm×74 mm,位于腹膜后和
左髂窝,密度均匀无坏死,腹主动
脉推压移位,左肾盂积水

图2 化疗前CT静脉期显像,左肾盂积水
血清肿瘤标志物检查示甲胎蛋白(AFP)、癌胚抗原(CEA)、癌抗原(CA)199、CA 125、CA 153等均正常。
介入超声引导下行腹膜后肿块穿刺活检。第一次穿刺活检,送检组织在显微镜下几乎全部为坏死成分,仅残存少许恶性肿瘤小圆细胞,因细胞量少无法确定病理类型。第二次穿刺活检,组织切片显微镜下见大量胶原纤维增生,肿瘤细胞灶性分布,细胞幼稚、核深染,表达上皮、间叶及神经源性多系分化免疫核型:细胞角蛋白(CK)灶性++,结蛋白(desmin)++,波形蛋白(vimentin)+,S100+,突触素(Syn)++,CD99+/-(图5~9)。
诊断
经腹部软组织肉瘤多学科协作组(MDT)专家讨论,根据病理考虑高度恶性小圆细胞软组织肉瘤,横纹肌肉瘤或促结缔组织增生性小圆细胞肿瘤皆有可能。
治疗
上述两种类型软组织肉瘤均对化疗敏感,而患者肿瘤巨大、包绕和压迫血管,手术暂无法达到根治切除目的,而且可能带来巨大创伤,鉴于此,行异环磷酰胺联合多柔比星方案化疗。
患者化疗第1周期后左下肢肿胀及酸痛好转。第2周期化疗后左下肢水肿再次加重,下肢深静脉超声检查显示左下肢深静脉血栓形成,给予华法林、阿司匹林、蚓激酶等治疗后水肿明显减轻。第3周期化疗后,复查CT显示病灶明显缩小。第4周期化疗后(图3、4),重复CTA检查并再次提请MDT讨论下一步治疗方案:①是继续化疗、手术还是放疗;②手术的可行性、时机及手术计划;③放疗应在术前还是术后进行?

图3 化疗4周期后动脉期显像,肿块
大小70.1 mm×102.3 mm

图4 化疗4周期后静脉期显像,肿块
明显囊变、坏死,腹主动脉受压消
失,肠系膜上动、静脉显示良好
MDT讨论荟萃
软组织肉瘤是一种间叶源性、高度异质性的少见肿瘤,在所有恶性肿瘤中的比例不到1%,可发生于全身各部位除骨和软骨以外所有的结缔组织。位于腹膜后的软组织肉瘤,发现时往往瘤体较大、侵犯较广、周围血管神经较多,手术难度大,不易切干净,需要专门从事肉瘤研究的外科、病理科、放射科、肿瘤放化疗科专家组成的多学科团队协作,进行规范化诊断并制定合理的治疗方案。
应明确组织学诊断
根据美国国立综合癌症网络(NCCN)指南建议,治疗前应尽可能明确组织学诊断及分级,特别是腹膜后或腹腔肿块,若影像学上判断为不能切除的肿瘤并拟行术前新辅助放化疗,或怀疑为淋巴瘤、生殖细胞肿瘤或其他肿瘤转移时,CT、超声引导下空心针穿刺或腹腔镜下活检对于明确病理诊断具有重要意义。
软组织肉瘤主要有小圆细胞、梭形细胞和多形性三种细胞形态学类型,有些肿瘤还含有上皮样细胞组成的区域。形态学上呈小圆细胞的亚型,如尤文肉瘤家族、腺泡状横纹肌肉瘤、促结缔组织增生性小圆细胞肿瘤、分化差的滑膜肉瘤、间充质软骨肉瘤等,具有侵袭性强、预后差、对化疗较敏感等临床特点,化疗是除手术和放疗外重要的治疗手段。
横纹肌肉瘤 根据该患者肿瘤形态学及免疫核型特点,首先考虑横纹肌肉瘤(RMS)。
RMS是一种具有骨骼肌分化倾向的原始间叶细胞恶性肿瘤,为儿童和青少年最常见的软组织肉瘤类型,病理组织学上有胚胎性、腺泡状和多形性等三种主要亚型,成人一般为多形性。镜下可见恶性细胞有向骨骼肌分化的形态特征和免疫组化表现,desmin和成肌蛋白(myogenin)染色阳性,其中myogenin具有特异性诊断意义。
该患者的组织学特点为大量纤维组织增生、肿瘤细胞表达多系分化的免疫核型,故考虑其不符合典型的横纹肌肉瘤病理特征。
促结缔组织增生性小圆细胞肿瘤 另一种也是由小圆细胞组成的高度恶性软组织肉瘤是促结缔组织增生性小圆细胞肿瘤(DSRCT)。
DSRCT临床上往往表现为腹腔内坚硬、多结节性巨大包块,可有囊性区域,病理学上典型表现为大小不一、外形不规则的小圆细胞巢,伴周围大量致密纤维结缔组织增生,肿瘤细胞具有上皮、间叶和神经内分泌多向分化的免疫表型,与该患者有相似的表现。
但DSRCT发病率低,以儿童和青少年、男性患者为主,发病年龄和性别方面与该患者不符。DSRCT一般不表达肌源性标志物如myogenin和肌红蛋白(Myo)D1,细胞遗传学检测有特异性的t(11,22)(p12,q12)易位,采用逆转录聚合酶链式反应(RT-PCR)方法可检测出WT1-EWS融合性信使RNA(mRNA)。如可取得足够的组织学标本,通过进一步相关免疫组化或分子生物学检测可与横纹肌肉瘤鉴别。与RMS一样,DSRCT对化疗敏感。
还有一些其他需要鉴别诊断的小圆细胞肿瘤,包括恶性淋巴瘤、骨外尤文肉瘤/外周原始神经外胚层肿瘤(PNET)、圆细胞脂肪肉瘤、成神经细胞瘤、神经内分泌肿瘤等,目前病理结果基本可排除这些肿瘤。
手术切除须看准时机
软组织肉瘤的主要治疗手段是手术切除。美国NCCN指南强调,软组织肉瘤的外科治疗应遵循以下原则:①尽可能获得理想的手术切缘;②尽量保留未受侵犯的重要血管神经或脏器如骨、关节等;③如肿瘤累及重要血管、神经,外科不能保证彻底根治时,可根据病理类型考虑术前化放疗降期,再判断手术的可行性。对于有症状的患者,姑息减瘤术也是一种治疗选择,而对无症状的患者可采取观察等待的策略。
该患者4周期化疗后,CT显示其肿瘤从化疗前的126 mm×74 mm缩小至70.1 mm×102.3 mm,腹主动脉受压消失,肠系膜上动静脉显示良好,为手术切除创造了条件。手术的难点在于血管、肾脏的处理。血管外科专家认为腹主动脉主要为受压推移而非受侵,由于主动脉外膜厚,术中可剥离,其他受累血管的处理如髂血管重建、肠系膜下动脉结扎等在技术上可行。普外科专家认为,肠系膜下动脉切除一般不影响肠管的血供,若乙状结肠系膜同时受侵须行部分肠段切除。泌尿外科专家意见为,患者肿瘤恶性程度高,虽然目前CT上显示左输尿管为受压表现,但不能排除侵袭受累的可能,且左肾功能已经减退,可行左肾联合左输尿管切除,但术前须通过同位素肾图检查了解及评价对侧肾功能。
综合上述讨论,MDT意见为:患者虽在化疗后已具有一定的手术条件,但目前手术风险仍较大,如何掌握最佳手术时机仍值得探讨;目前可以手术,也可以继续原方案化疗,在密切影像学随访认为无法进一步获益的时候再行手术切除,术后辅助放疗。[4320201]



图5 苏木素-伊红(HE)染色,低倍镜 图6 免疫组化(IHC)示desmin阳性 图7 IHC示Syn阳性
下见大量胶原纤维增生及少量灶
性分布的肿瘤细胞

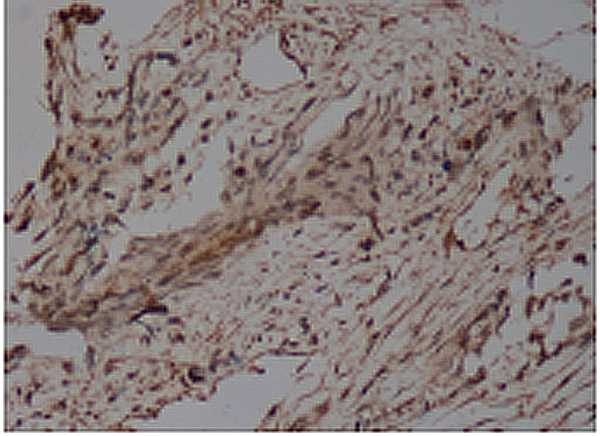
图8 IHC示S100 图9 IHC示CD99弱阳性
(复旦大学附属中山医院腹部软组织肉瘤MDT协作组 陆维祺 周宇红 蒋亚平 纪元 侯英勇 严福华 张立 史振宇)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







已阅,受益匪浅。
47
#软组织#
29
#多学科#
45
#MDT#
27
#腹膜#
32