JACC:主血管支架置入后侧枝闭塞的预测因素
2013-08-19 高晓方 译 cmt
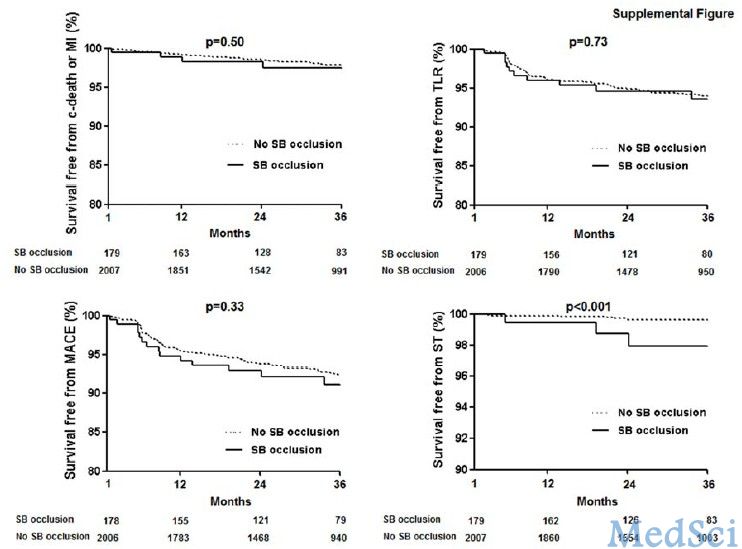
韩国一项研究表明,侧枝血管造影表现、近端主血管(MV)狭窄和临床表现为MV支架置入后侧枝闭塞的预测因素;大侧枝闭塞与不良临床转归相关。论文8月在线发表于《美国心脏病学会杂志》(J Am Coll Cardiol)。【原文下载】 此项研究共纳入2227例因冠脉分叉病变而行药物洗脱支架PCI治疗的患者。以心肌梗死溶栓(TIMI)血流分级<3定义MV支架置入后侧枝闭
韩国一项研究表明,侧枝血管造影表现、近端主血管(MV)狭窄和临床表现为MV支架置入后侧枝闭塞的预测因素;大侧枝闭塞与不良临床转归相关。论文8月在线发表于《美国心脏病学会杂志》(J Am Coll Cardiol)。【原文下载】
此项研究共纳入2227例因冠脉分叉病变而行药物洗脱支架PCI治疗的患者。以心肌梗死溶栓(TIMI)血流分级<3定义MV支架置入后侧枝闭塞。评估侧枝闭塞的预测因素和临床转归。
结果显示,共有187例(8.4%)患者出现侧枝闭塞。在多变量分析中,侧枝闭塞的独立预测因素为术前侧枝狭窄≥50%(比值比[OR] 2.34)、近端主血管狭窄≥50%(OR 2.34)、侧枝病变长度(OR 1.03)和急性冠脉综合征(OR 1.53)。在187例侧枝闭塞患者中,血流自主恢复和介入恢复者分别为26(13.9%)和103例(55.1%)。侧枝保护性导丝与血流恢复相关。侧枝闭塞患者更有可能出现心源性死亡或心肌梗死(校正危险比2.34)。
原始出处:
Joo-Yong Hahn; Woo Jung Chun; Ji-Hwan Kim; Young Bin Song; Ju Hyeon Oh; Bon-Kwon Koo; Seung Woon Rha; Cheol Woong Yu; Jong-Sun Park; Jin-Ok Jeong; Seung-Hyuk Choi; Jin-Ho Choi; Myung-Ho Jeong; Jung Han Yoon; Yangsoo Jang; Seung-Jea Tahk; Hyo-Soo Kim; Hyeon-Cheol Gwon.Predictors and Outcomes of Side Branch Occlusion after Main Vessel Stenting in Coronary Bifurcation Lesions: Results from the COBIS (COronary BIfurcation Stenting) II Registry ONLINE FIRST.J Am Coll Cardiol. 2013;():. doi:10.1016/j.jacc.2013.07.041 【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#JACC#
37
#预测因素#
31
#ACC#
40