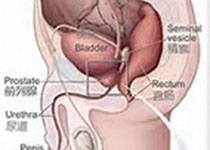
Prostate Cancer P D:总量和酒精饮料摄入与侵入性前列腺癌风险
2017-04-30 AlexYang MedSci原创
酒精饮料中的乙醇是知名的致癌物质,但是它与侵入性前列腺癌(APC)的关系却并不知晓。近期的一些研究指出,APC患病率的一定程度增加与大量酒精摄入有关系,但是对酒精饮料的类型仍旧不清楚。最近,研究人员利用案例-对照设计和自我陈述调查就APC与酒精摄入频率和量的关系进行了研究,酒精摄入超过两年的优先考虑,并且APC包括高级和晚期两种阶段。更多的是,研究人员描述了酒精饮料啤酒、红酒、白酒和烈酒与APC的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Prostate Ca#
43
#前列腺癌风险#
43
#侵入性#
38
#癌风险#
34
#ROS#
40
#PRO#
32