妊娠糖尿病(GDM)血糖监测及控制目标
2012-01-25 MedSci MedSci原创
血糖监测是血糖控制措施安全、有效进行的前提,包括即刻血糖监测、动态血糖监测(CGM)。 妊娠糖尿病(GDM)患者常用、可行的方法是自我指尖血糖监测,建议开始时用七点法(三餐前0.5小时、三餐后2小时和夜间睡前共7次)。注意:出现头晕、眼花不适时,应考虑低血糖可能,立即测血糖并及早处理。血糖达标、稳定时可减少监测次数至每天4次。 即刻血糖监测是瞬时血糖值,而CGM可反映24小时
血糖监测是血糖控制措施安全、有效进行的前提,包括即刻血糖监测、动态血糖监测(CGM)。
妊娠糖尿病(GDM)患者常用、可行的方法是自我指尖血糖监测,建议开始时用七点法(三餐前0.5小时、三餐后2小时和夜间睡前共7次)。注意:出现头晕、眼花不适时,应考虑低血糖可能,立即测血糖并及早处理。血糖达标、稳定时可减少监测次数至每天4次。
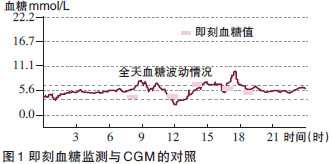
即刻血糖监测是瞬时血糖值,而CGM可反映24小时血糖变化规律(图1),能够发现即刻血糖监测未知的餐后高血糖和夜间低血糖,并可反映饮食、运动、药物等对血糖的影响,是即刻血糖监测的有力补充,已被中国动态血糖监测临床应用指南(2009年版)推荐常规用于GDM血糖管理。

附:
妊娠糖尿病(GDM)患者及早确诊及治疗后,母婴预后明显改善、并发症明显减少。以自我血糖监测、饮食控制、胰岛素治疗和各专科医生合作而制订的强化治疗方案是降低GDM母婴并发症、改善预后的关键。
营养治疗指南

药物治疗
患者一旦确诊GDM即应开始饮食控制及运动治疗,若经1~2周血糖仍不能达标,则须药物治疗。
胰岛素不能通过胎盘进入胎儿体内直接导致胎儿畸形或低血糖发生,因此,目前仍建议以人胰岛素治疗为主。胰岛素应用根据患者血糖轮廓图谱确定,仅餐后血糖升高者,可在相应餐前给予适量短效胰岛素;如果空腹血糖升高,可在睡前给予中效胰岛素治疗;有些患者可选择预混胰岛素。
此外,近年来口服降糖药物治疗GDM报道中研究最多的是格列本脲和二甲双胍。有研究表明,格列本脲和二甲双胍与胰岛素一样,都能有效控制GDM患者血糖,且对妊娠结局影响与胰岛素无明显差别。但需要注意,目前尚无指南推荐上述口服降糖药物作为治疗GDM的最佳选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#GDM#
32
#血糖监测#
48
#控制目标#
40