CID:脑膜炎球菌B疫苗对青少年侵袭性脑膜炎的影响。
2021-09-29 从医路漫漫 MedSci原创
由脑膜炎奈瑟菌引起的侵袭性脑膜炎球菌病(IMD)仍然是世界范围内发病率和死亡率的重要原因。
背景:自2017年起,在南澳大利亚开展了一项全州范围的随机试验,以评估脑膜炎球菌B疫苗4CMenB对青少年咽部脑膜炎奈瑟菌携带的影响。由脑膜炎奈瑟菌引起的侵袭性脑膜炎球菌病(IMD)仍然是世界范围内发病率和死亡率的重要原因。在澳大利亚、欧洲、北美和南美洲,大部分IMD病例是由B群脑膜炎引起的。高中生在2017年(干预)或2018年(对照)随机接种疫苗。在这项研究中,我们报道了4CMenB疫苗对南澳大利亚16- 19岁青少年B血清群侵袭性脑膜炎球菌病(IMD)的影响。
方法。这项对血清组B IMD病例的观察性时间序列分析比较了试验开始前14年(2003-2016年)与2017年接种4CMenB疫苗后2年的青少年队列。
结果。在南澳大利亚州,大约62%的10年级和11年级学生(15-16岁)参加了试验。总共有30 522名10-12岁的学生接受了至少1剂4CMenB。从2003年到2016年,南澳大利亚州16- 19岁青少年中血清B组IMD病例的数量平均每年增加10%(95%置信区间[CI], 6%-15%, P < .001), 2015年达到峰值,10例。血清组B IMD病例在2017-2018年减少到5例,在2018-2019年减少到1例,分别低于9.9(95%预测区间[PI],3.9-17.5)和10.9 (95% PI, 4.4-19.1)的预期数字。这意味着血清B组IMD病例总数减少了71% (95% CI, 15%-90%,P =0 .02)。在接种疫苗的青少年中没有血清组B型IMD病例。
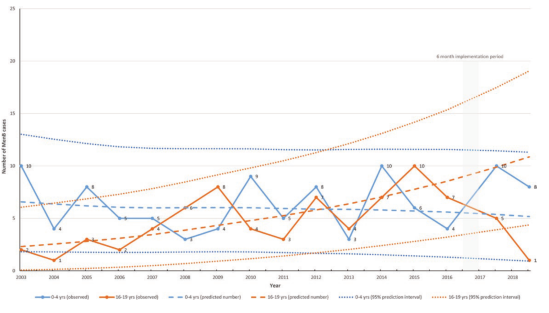
图 根据符合研究前阶段(2003-2016)并延续4CMenB至高中阶段(2017-2018年至2018-2019年)的趋势线,在南澳大利亚观察和预测B组侵袭性脑膜炎球菌病(IMD)病例,0-4岁和16-19岁年龄组的预测间隔为95%。缩写:MenB,脑膜炎球菌B。
结论。在南澳大利亚,青少年接种4CMenB疫苗与B组脑膜炎球菌病的减少有关。
原文出处:
McMillan M, Wang B, Koehler AP, et al,Impact of Meningococcal B Vaccine on Invasive Meningococcal Disease in Adolescents.Clin Infect Dis 2021 07 01;73(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#CID#
36
很好的医学知识,感谢分享
87
#侵袭性#
45
谢谢分享
75
学习了
0