NEJM:阿尔茨海默病新药Solanezumab III期临床试验失败
2014-02-08 zzymm dxy
β-淀粉样蛋白(Aβ)在大脑皮层及海马沉积是阿兹海默氏症的病理改变之一。Solanezumab,一种人源化单克隆抗体,可选择性结合可溶性Aβ,临床前研究表明它能促进大脑Aβ排泄。 为此,礼来(Eli Lilly)开展了Solanezumab 的两项III期临床研究,令人遗憾的是均以失败告终,相关结果发表在2014年1月23日的NEJM上。 该III期临床试验为随机双盲对照研究,以轻到中
β-淀粉样蛋白(Aβ)在大脑皮层及海马沉积是阿兹海默氏症的病理改变之一。Solanezumab,一种人源化单克隆抗体,可选择性结合可溶性Aβ,临床前研究表明它能促进大脑Aβ排泄。
该III期临床试验为随机双盲对照研究,以轻到中度阿兹海默氏症患者为研究对象,包括EXPEDITION 1(纳入患者1012例)和EXPEDITION 2(1040例)。研究对象随机分为安慰剂组及solanezumab药物组(400mg 静脉用药),每4周一次给药,为期18个月。(图1)
图1.EXPEDITION 1和EXPEDITION 2研究对象入组及试验完成情况
主要终点事件为80周后以下相关评分的变化:11项阿兹海默氏症认知评分(ADAS-cog11;0到70分, 得分越高认知障碍越重)以及阿兹海默氏症协作研究日常生活能力评分(ADCS-ADL;0到78分,得分越低功能越差)。
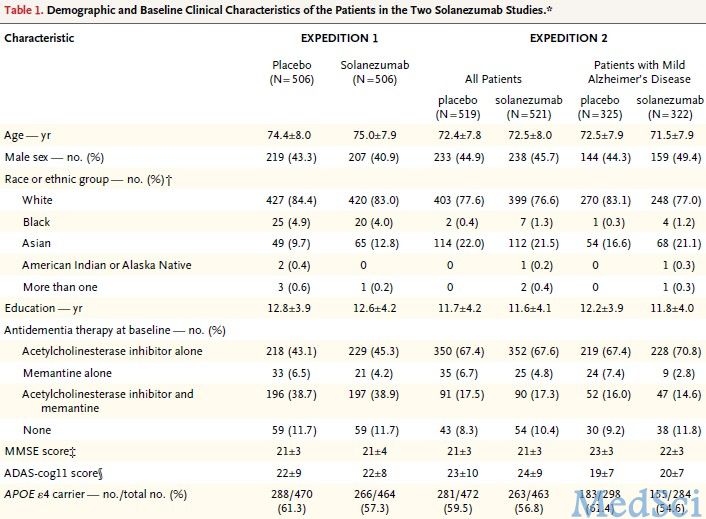
分析完EXPEDITION 1数据后,将EXPEDITION 2轻度阿兹海默氏症患者的主要终点事件修正为14项阿兹海默氏症认知评分变化(ADAS-cog14;0到90分, 得分越高认知障碍越重)。(表1)
表1.EXPEDITION 1和EXPEDITION 2研究对象一般基线信息
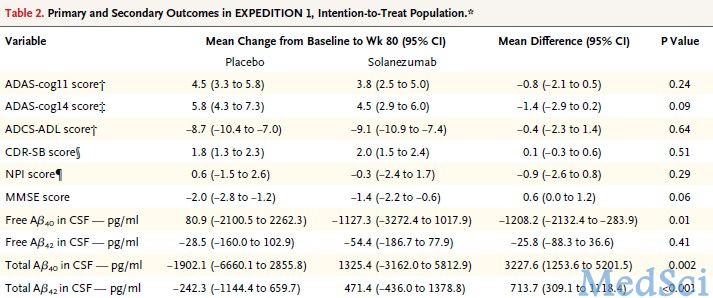
两项III期临床试验结果均表明solanezumab不能明显改善患者的主要终点事件。EXPEDITION 1研究显示,与基线相比,80周后ADAS-cog11评分变化的组间差异(药物组减安慰剂组)为-0.8分,而ADCS-ADL组间差异为-0.4分。(表2)
表2.EXPEDITION 1研究结果
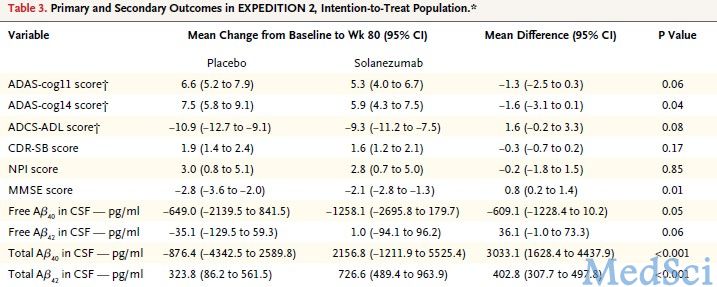
在EXPEDITION 2,ADAS-cog11评分变化的组间差异为-1.3分,ADCS-ADL组间差异为1.6分(表3)。
表3.EXPEDITION 2研究结果
轻度阿尔茨海默氏症患者ADAS-cog14评分变化的组间差异为-1.7分,中度阿尔茨海默氏症患者组间差异为−1.5分(表4)。
表4.EXPEDITION 2轻、中度患者亚组分析结果
总之,该III期临床试验表明Solanezumab不能改善阿兹海默氏症患者认知或者生活能力。但是,在轻度或者无临床症状但是已有证据表明Aβ沉积的阿兹海默氏症患者,Solanezumab疗效如何,仍需更深入的研究。
原文出处:
Doody RS, Thomas RG, Farlow M, Iwatsubo T, Vellas B, Joffe S, Kieburtz K, Raman R, Sun X, Aisen PS, Siemers E, Liu-Seifert H, Mohs R; Alzheimer's Disease Cooperative Study Steering Committee; Solanezumab Study Group.Phase 3 trials of solanezumab for mild-to-moderate Alzheimer's disease.N Engl J Med. 2014 Jan 23;370(4):311-21. doi: 10.1056/NEJMoa1312889.【原文下载】
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#阿尔茨#
38
#I期临床试验#
38
#Solanezumab#
41
#III#
31
#mAb#
30
#I期临床#
22
#II期临床试验#
32
#阿尔茨海#
30
#阿尔茨海默#
34
#II期临床#
29