Bioactive Materials:程柯、王少为团队开发新型多功能避孕凝胶
2020-12-24 生物探索 生物探索
新型多功能避孕水凝胶能够同时实现避孕、预防性传播疾病、以及改善雄性性欲及勃起三大功能。
传统的的避孕方式包括安全期避孕、口服避孕药、宫内节育器以及避孕套。但安全期避孕的失败率高达50%以上,所以并不安全;口服避孕药虽避孕效果好,但如果女性漏服,不仅仅要面对失败风险,更多女性还会出现因激素撤退而导致的异常子宫出血;宫内节育器需要侵入性手术放置及取出,不方便操作,且一旦出现避孕失败就会面临带器妊娠,属于极高危的妊娠合并症;避孕套作为最常用的避孕方法,但是众多男性认为其降低性交快感从而拒绝使用,且仍有一定几率因脱落或破损而导致意外怀孕。
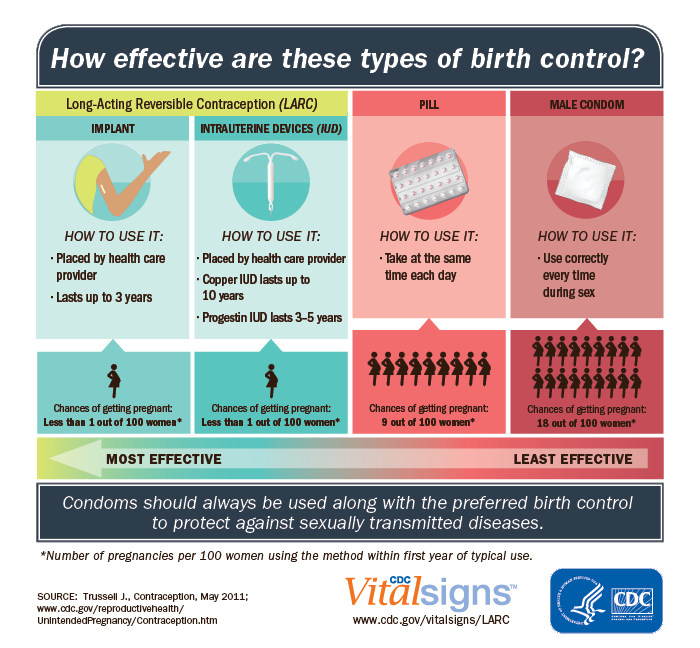
目前常用的避孕方式 (来源:cdc.gov)
近日,北卡罗来纳州立大学和北卡大学教堂山分校的程柯教授与北京医院妇产科主任医师王少为教授合作,带领团队在知名生物材料杂志Bioactive Materials杂志上发表文章A Trifunctional Contraceptive Gel Enhances the Safety and Quality of Sexual Intercourse(共同第一作者谢孟杰,李俊朗,及张思辰)。该研究使用FDA批准的生物材料及药物,采用高分子水凝胶为载体,以替诺福韦(Tenofovir)、棉子酚(Gossypol-acetic acid) 、硝酸甘油(Nitroglycerin)为成分,设计并生产出同时实现避孕、预防性传播疾病、以及改善雄性性欲及勃起三大功能的新型多功能避孕水凝胶——“特坚安”(TGN, 取自三种药物的首字母)。
该研究测试了TGN水凝胶的结构及稳定性,证明其常温状态下稳定,呈胶质状态,粘附性高,易于保存和运输,且使用时不易流失。TGN的微酸性特性更是契合女性阴道内环境,不会导致阴道内环境失衡诱发阴道炎。
体外实验结果证明,TGN水凝胶能够快速并有效杀死活力在90%以上的猪精子,且不破坏健康的阴道上皮细胞。将TGN凝胶加入与荧光慢病毒共培养的阴道上皮细胞中,2小时内,在共聚焦显微镜下观察到TGN凝胶能够有效抑制病毒对细胞的转染 (Fig. 3),显示其具有预防病毒感染阴道的潜能。这一功效,对预防HIV性传播、女性HPV感染及宫颈病变甚至宫颈癌的发生都具有重大意义。
在进一步的动物试验中,研究者给动情期内雌性大鼠阴道内涂抹TGN水凝胶并将其与发情期的雄鼠同笼,以涂抹PBS或市场上在售的其他类型凝胶作为对照。结果发现,涂抹TGN水凝胶的雌鼠无一妊娠,而涂抹PBS的雌鼠全部妊娠,涂抹其他类型凝胶的雌鼠妊娠率亦高于涂抹TGN水凝胶的雌鼠,有力证明了TGN水凝胶的避孕功效。
研究者还发现,将TGN水凝胶涂抹在雄性大鼠的生殖器上,能够增加雄鼠的勃起功能,其主动与雌鼠的交配次数也有显着增加,证明其有望增强男性的性欲及勃起功能。
总的来说,新开发的多功能避孕凝胶“特坚安”(TGN)在有效发挥避孕功能的同时,兼具抗病毒感染和增强雄性勃起功能的效果。程柯教授表示,虽然本项目在动物试验中取得了较为理想的成果并展示出一定的转化潜能,任何一项医疗器械在批准上市前都需要经过大量的临床试验和质量检测才能保证其安全性、有效性。团队希望经过努力为未来的避孕市场提供了新的思路和产品。目前,北卡州立大学已经针对TGN凝胶的组分和生产工艺申请了全球专利保护,未来将选择合适的商业合作伙伴进行下一步开发。
通讯作者:程柯教授

通讯作者:王少为主任医师
原始出处:
Mengjie Xie, et al. A trifunctional contraceptive gel enhances the safety and quality of sexual intercourse. Bioactive Materials, 2021, Pages 1777-1788.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#active#
36
#Bio#
31
#凝胶#
29
好文章!
79