J Hematol Oncol:癌症患者接种SARS-COV2疫苗后的血清学反应
2022-03-08 从医路漫漫 MedSci原创
由严重急性呼吸系统综合症冠状病毒 2 (SARS-CoV-2) 引起的2019年冠状病毒病 (COVID-19) 大流行持续存在,世界又迎来了全球卫生紧急事件的一年。
背景:由严重急性呼吸系统综合症冠状病毒 2 (SARS-CoV-2) 引起的2019年冠状病毒病 (COVID-19) 大流行持续存在,世界又迎来了全球卫生紧急事件的一年。过去一年的广泛研究表明,老年患者以及患有肥胖症、糖尿病和癌症等既往疾病的患者更容易感染 SARS-CoV-2 并发展为危及生命的肺炎。在美国,大约 9.5% 的成年人已经或曾经诊断出任何类型的癌症,每 3 名成年人中就有 1 人将在其一生中的某个时间点被诊断出患有癌症。保护癌症患者的健康和安全至关重要,并被视为 COVID19 大流行期间的主要优先事项。
梅塔等人报道,癌症患者的年龄增加、合并症和体能状况不佳与 COVID-19 预后不良有关。与实体癌患者相比,血液系统癌症患者的病死率 (CFR) 更高(37% 对 25%)。这些数据表明需要对癌症患者采取预防策略,这些患者通常由于其潜在的疾病状态和使用化学疗法、放射疗法、骨髓或干细胞移植和/或免疫疗法而受到免疫抑制。由于缺乏针对 COVID-19 的有效治疗方法,包括疫苗接种在内的预防策略对于降低风险和死亡率至关重要。针对 COVID-19 的疫苗开发迅速,新出现的数据表明,基于 mRNA 的 COVID-19 疫苗在普通人群中是有效和安全的。然而,COVID-19 疫苗对癌症患者的疗效尚不清楚,因为活动性癌症患者或接受免疫抑制治疗的患者被排除在监管疫苗试验之外。目前指南建议癌症患者应接种 SARS-CoV-2 疫苗,只要疫苗的任何成分都没有禁忌。来自其他疫苗可预防疾病的数据表明,接受细胞毒性化疗的实体癌患者对疫苗的体液反应减弱。最近的研究报道,与实体瘤患者相比,血液系统恶性肿瘤患者,尤其是接受抗 CD20 治疗或有干细胞移植史的患者,对 BNT162b2 或 mRNA1273 SARS-CoV-2 疫苗的免疫原性减弱。调查 COVID-19 疫苗在癌症患者中的有效性的其他研究是有限的,而且大多数都是小样本。
更好地了解 COVID-19 疫苗在癌症患者中的整体有效性将改善临床护理并保护这些弱势患者群体。在这项系统评价和荟萃分析中,我们的目的是整合研究结果,以确定癌症患者对 COVID-19 疫苗接种的血清学反应率。
目的:癌症患者患 2019 年冠状病毒病 (COVID-19) 的风险增加,并且对各种疫苗的反应减弱。这项荟萃分析旨在评估癌症患者对 COVID-19 疫苗接种的血清学反应。
方法:在 2021 年 8 月 1 日系统地搜索电子数据库,以查找报告癌症患者对 COVID-19 疫苗的血清学反应的研究。随机效应模型用于实现汇总的血清学反应率和优势比 (OR)。
结果:我们分析了 16 项观察性研究,共有 1453 名癌症患者。大多数研究使用 mRNA 疫苗(BNT162b2 或 mRNA-1273)。在单剂和两剂 COVID-19 疫苗后实现血清学应答的患者比例分别为 54.2%(95% 置信区间 [CI] 41.0–66.9)和 87.7%(95% CI 82.5–91.5)。与实体器官癌患者相比,血液系统癌症患者在第二剂疫苗后的反应率较低(63.7% vs. 94.9%),这归因于与某些疾病(慢性淋巴细胞白血病、淋巴瘤)相关的低反应率和疗法(抗 CD20、激酶抑制剂)。与对照患者相比,在接种一剂和两剂疫苗后,较低比例的癌症患者获得了血清学应答(分别为 OR0.073 [95% CI 0.026–0.20] 和 0.10 [95% CI 0.039–0.26])。

图 1 接种一剂疫苗后血清学反应的 Meta 分析。 B 两剂疫苗后血清学反应的荟萃分析
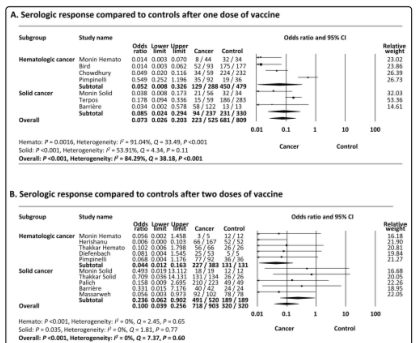
图2 与对照组相比,接种一剂疫苗后血清学反应的荟萃分析。 B 两剂疫苗后血清学反应与对照相比的荟萃分析
结论:癌症患者,尤其是血液 B 细胞恶性肿瘤患者,对 COVID-19 疫苗的血清学反应较低。结果表明,癌症患者应继续遵循安全措施,包括在接种疫苗后戴上口罩,并建议需要额外的预防策略。
原文出处: Sakuraba A, Luna A, Micic D,Serologic response following SARS-COV2 vaccination in patients with cancer: a systematic review and meta-analysis.J Hematol Oncol 2022 02 05;15(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#SARS-CoV#
47
#Oncol#
38
#癌症患者#
44
#EMA#
33
#SARS#
40
#血清学#
51