Nat rev Cardiol:心脏磁共振在心脏淀粉样变中的应用价值
2014-03-14 伊文 丁香园
甲状腺素运载蛋白介导的心脏淀粉样变(ATTR)是一种致命性的疾病,其发病机制为甲状腺素运载蛋白野生型或突变型以淀粉样形式沉淀于心脏。尽管针对这种疾病的特定治疗正在出现,但疾病诊断以及疾病进展监测仍存在很大挑战。【原文下载】 来自英国的Fontana教授称:“淀粉样变进展期时心电图、超声心动图、生物标记物等指标有所改变,但这些指标可能会受到左心室肥厚等混杂因素的干扰。”2013年,研究报道
甲状腺素运载蛋白介导的心脏淀粉样变(ATTR)是一种致命性的疾病,其发病机制为甲状腺素运载蛋白野生型或突变型以淀粉样形式沉淀于心脏。尽管针对这种疾病的特定治疗正在出现,但疾病诊断以及疾病进展监测仍存在很大挑战。【原文下载】
来自英国的Fontana教授称:“淀粉样变进展期时心电图、超声心动图、生物标记物等指标有所改变,但这些指标可能会受到左心室肥厚等混杂因素的干扰。”2013年,研究报道心脏磁共振(CMR)T1像有助于监测心脏AL(免疫球蛋白轻链)淀粉样变进展。Fontana教授等进一步评估了CMR是否可以用于监测ATTR。
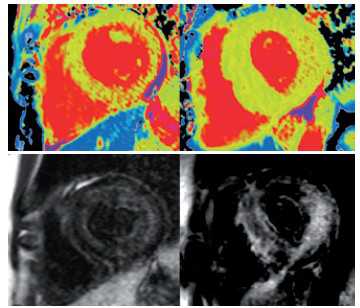
相比健康人群(52名)、心肌肥厚患者(46名)以及TTR基因病理性突变但无心脏淀粉样沉淀证据的患者(8名),85名ATTR患者T1值升高。尽管T1像在诊断ATTR和AL淀粉样变的准确性相似,ATTR T1值不如AL淀粉样变高(79名)。
研究人员对该结果表示惊讶,因为ATTR室壁明显厚于AL淀粉样变。心脏淀粉样变越严重,T1值越大,与其它ATTR或AL淀粉样变测量保持一致。研究人员总结道:“心肌T1成像可以监测ATTR,在诊断和监测ATTR和AL淀粉样变方面能力相似。”
在北美的一项研究中,共纳入90名可疑心脏淀粉样变(不同病因)和64名高血压左室肥厚患者,并行CMR检查(采用修改的T1成像方案)。53%可疑心脏淀粉样变患者呈现弥漫性高密度影,而高血压心室肥厚患者中无1例呈现高密度影。另外12%可疑心脏淀粉样变患者呈现散在高密度像,而在高血压心室肥厚患者,这一比例为6%。随访29个月发现弥漫性或任何高密度显影均增加全因死亡率。
来自英国的另外一个研究组也研究了CMR在心脏淀粉样变中的使用,特别关注CMR在ATTR和AL淀粉样变显像上是否不同。Dungu博士等回顾比较了51名ATTR患者和46名AL淀粉样变患者的钆对比剂延迟强化(LGE)显影。几乎所有ATTR和AL淀粉样变患者(除了1名)呈现LGE显影。但是,ATTR患者LGE显影范围更广:所有患者右室均显影(AL淀粉样变为72%),90%透壁显影(AL淀粉样变仅为37%)。
研究人员为可疑心脏淀粉样变患者设立了评分标准,即QALE评分。评分包括心底部、室间隔、心间部LGE信息,并且是淀粉样变类型的独立预测因子。整合年龄、室间隔厚度和QALE评分信息的的logistic回归分析对诊断ATTR的敏感度和特异性分别是87%和96% 。
Dungu博士等的研究指出,T1成像可能成为衡量淀粉样沉积导致的间质扩张程度的金标准,但该临床操作可能不适用于所有患者。同时,他们总结道CMR LGE评分能够增强多数病人的治疗水平,但是由于上述研究均为回顾性研究,尚缺少前瞻性队列研究的评估,因此,不能取代活检(目前诊断金标准)作为淀粉样变诊断的金标准。
原始出处:本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Nat#
35
#Cardiol#
33
#心脏淀粉样变#
49
#磁共振#
36
#心脏磁共振#
41
#淀粉样变#
32