Cell子刊:同样是胖子为何有人不得糖尿病?
2016-11-06 佚名 生物谷
几年以前,科学家们就已经发现有些瘦人最终也会得糖尿病,而一些比较胖的人反而能一直保持健康。现在来自犹他大学健康学院的科学家们发现了这一谜题的一个可能答案:一类具有毒性的脂肪代谢产物——神经酰胺——可能会让人易患2型糖尿病。相关研究结果发表在国际学术期刊Cell Metabolism上,该研究发现神经酰胺的积累会影响脂肪组织的正常功能。当人们吃的过多,体内就会产生过量的脂肪酸,有些脂肪酸能够储存为甘
几年以前,科学家们就已经发现有些瘦人最终也会得糖尿病,而一些比较胖的人反而能一直保持健康。现在来自犹他大学健康学院的科学家们发现了这一谜题的一个可能答案:一类具有毒性的脂肪代谢产物——神经酰胺——可能会让人易患2型糖尿病。
相关研究结果发表在国际学术期刊Cell Metabolism上,该研究发现神经酰胺的积累会影响脂肪组织的正常功能。
当人们吃的过多,体内就会产生过量的脂肪酸,有些脂肪酸能够储存为甘油三酯,或者作为能量燃烧掉,而对于有些人来说,脂肪酸还会变成神经酰胺。当神经酰胺过量积累,脂肪组织停止正常工作,无法储存到脂肪组织中的脂肪就会进入血管系统和心脏还会对其他外周组织造成损伤。
该研究发现将过多的神经酰胺添加到人类脂肪细胞或小鼠体内会引起对胰岛素的反应出现迟钝,并进一步发展为能量消耗能力的损伤。小鼠也更容易发展为糖尿病和脂肪肝。
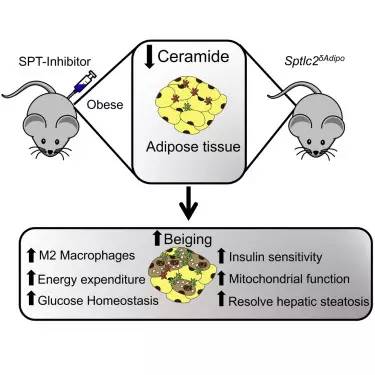
与之相反,研究人员在小鼠模型体内通过基因工程技术敲除了将饱和脂肪酸变成神经酰胺的关键基因结果发现降低小鼠脂肪组织内神经酰胺的含量能够保护小鼠避免出现胰岛素抵抗。
这些结果表明神经酰胺的积累可能增加糖尿病风险,而降低其水平则可以避免这种疾病。研究人员认为,这种现象在人类身上可能也同样存在。事实上通过对接受了减重手术的病人进行研究发现神经酰胺水平能够更好地预测糖尿病发生,甚至好于肥胖指标。虽然所有病人都处于肥胖状态,但那些没有患2型糖尿病的肥胖病人其脂肪组织内神经酰胺水平要低于诊断为2型糖尿病的肥胖病人。
研究人员还在寻找可能导致神经酰胺异常积累,并进一步发展为肥胖和2型糖尿病的基因突变。基于该研究,科学家们提出由于神经酰胺的积累,负责脂肪燃烧的棕色脂肪和米色脂肪组织可能失去了棕色脂肪的特性,甚至出现白色化,这进一步促进了导致疾病发生的一系列事件。
综上所述,该研究提示通过阻断脂肪组织内神经酰胺合成,或可防止2型糖尿病或其他代谢疾病的发生。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cell#
46
#CEL#
47
很好,不错,以后会多学习
62
很好,不错,以后会多学习
73
关注。谢谢编辑。值得学习。
63