Nature:癌细胞穿过血管壁发生转移机制被揭示
2016-08-12 佚名 生物谷
很多癌症仅当在体内其他地方形成转移瘤时才变成致命的危险。当单个癌细胞从原发性肿瘤中脱落下来,通过血液运行到达体内较远的部位时,继发性肿瘤(即转移瘤)就会形成。为了做到这一点,它们不得不穿过小血管壁。 如今,在一项新的研究中,来自德国马克斯普朗克心脏与肺部研究所、法兰克福大学的研究人员证实肿瘤细胞杀死血管壁中的特定细胞。这能够让它们离开血管和建立转移瘤,而且这种过程是由一种被称作死亡受体6(DR6

如今,在一项新的研究中,来自德国马克斯普朗克心脏与肺部研究所、法兰克福大学的研究人员证实肿瘤细胞杀死血管壁中的特定细胞。这能够让它们离开血管和建立转移瘤,而且这种过程是由一种被称作死亡受体6(DR6)的分子所促进的。相关研究结果发表在2016年8月11日那期Nature期刊上,论文标题为“Tumour-cell-induced endothelial cell necroptosis via death receptor 6 promotes metastasis”。
通过与来自德国科隆大学和海德堡大学的研究人员合作,马克斯普朗克心脏与肺部研究所药物学系主任Stefan Offermanns领导的一个研究团队成功地阐明了其背后的机制。研究人员首次利用体外培养的癌细胞开展实验,首先观察到单个肿瘤细胞如何杀死血管壁中的特定细胞,即血管内皮细胞。在实验室中,这种被称作坏死性凋亡(necroptosis)的过程能够让癌细胞穿过血管内皮细胞层。论文第一作者Boris Strilic说,“我们然后在小鼠体内开展的研究中证实同样的过程也在活的有机体中发生。”
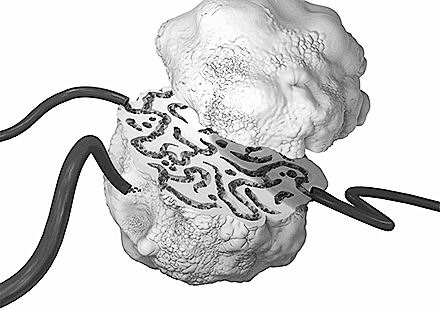
研究人员也发现血管内皮细胞自身也释放出宣告它们自己死亡的信号:这些血管壁细胞(即血管内皮细胞)在它们的表面上含有受体分子DR6。Strilic解释道,“当癌细胞与DR6接触时,癌细胞表面上的蛋白APP激活它。这标志着癌细胞开始攻击血管壁,最终导致血管壁细胞发生坏死性凋亡。”
细胞膜上的死亡受体
Offermanns团队随后证实在经过修饰的让DR6不再发挥功能的小鼠体内,更少的血管内皮细胞发生坏死性凋亡,因而也就导致更少的肿瘤细胞转移。Strilic说,“在阻断DR6或癌细胞蛋白APP后,也会发现这种效果,因而证实了我们之前的观察结果。”
然而,仍然并不完全清楚的是癌细胞是否直接通过血管壁中形成的空隙迁移出去,或者存在一种间接作用:“我们有证据证实当血管壁细胞死亡时,有更多的分子释放出来,这些分子使得癌细胞更容易从周围的区域渗透出去”,Offermanns说道。
Offermanns说,“这种机制可能是治疗或阻止所形成的转移瘤的一个大有希望的起点。”然而,首先还必需确定阻断DR6是否产生不想要的副作用。而且还必需确定这些观察结果在多大程度上适用于人体。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
26
#血管壁#
49
学习了,好
71
如果是这样那阻断抑制剂可能是比较好的设想
2
那我们可以通过拮抗或者先占据死亡受体从而达到延缓转移瘤的发生?可以这么想吗
73
继续关注
67
继续学习
77
继续关注
26
继续学习
22
学习了,期待进一步发展
22