Oncotarget:HADH表达下降通过激活Akt信号通路促进胃癌发展
2017-07-28 Emma MedSci原创
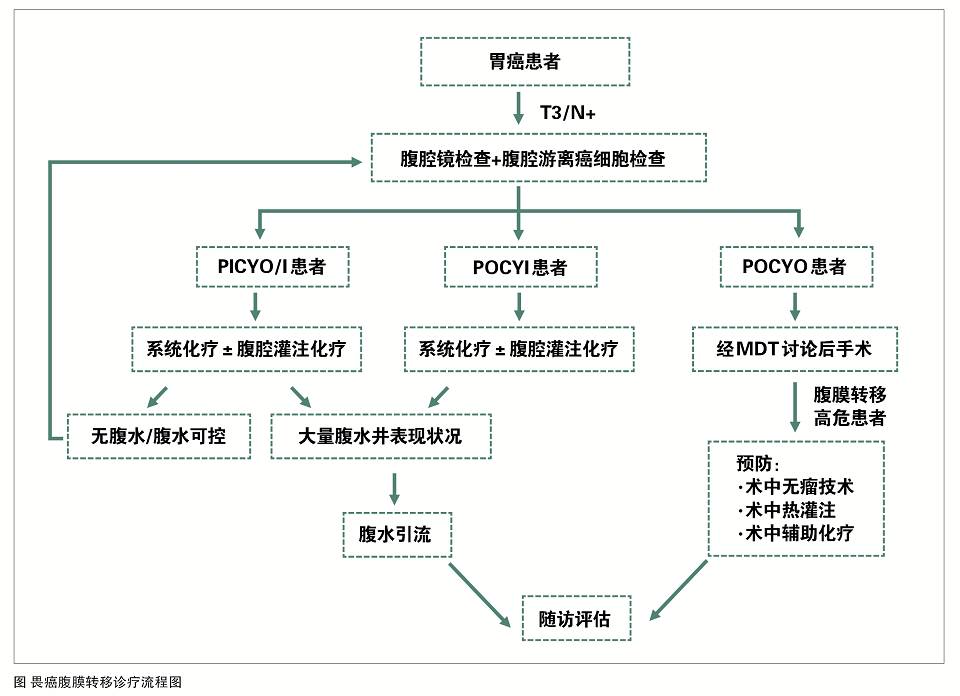
胃癌的扩散和转移途径有直接浸润、血行转移、腹膜种植转移以及淋巴转移,其中淋巴转移是胃癌的主要转移途径,进展期胃癌的淋巴转移率高达70%左右,早期胃癌也可有淋巴转移。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#target#
40
#Akt#
34
HADA表达下降.
72
HADH表达下降.
55
胃癌发展的促进.
52
HADH表达下降.
58
HADH表达下降促进胃癌发展.
61
HADH表达下降。
32
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
27
#信号通路#
31