Cell reports:Sirt1 N端结构域调控Srit1去乙酰化酶活性
2015-03-23 佚名 生物谷
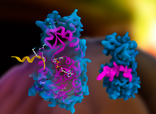
近日,来自美国华盛顿大学医学院的研究人员在国际期刊cell reports发表了他们的最新研究进展,他们发现去乙酰化酶Sirt1的N端结构域能够促进内源性Sirt1与NF-kB p65结合,执行去乙酰化酶活性。这项研究发现了调控Sirt1去乙酰化酶活性的新机制,具有一定意义。 研究人员指出,NAD+依赖性蛋白去乙酰化酶SIRT1通过对包括组蛋白和转录因子在内的多种蛋白进行去乙酰化,在调节代谢,应激
近日,来自美国华盛顿大学医学院的研究人员在国际期刊cell reports发表了他们的最新研究进展,他们发现去乙酰化酶Sirt1的N端结构域能够促进内源性Sirt1与NF-kB p65结合,执行去乙酰化酶活性。这项研究发现了调控Sirt1去乙酰化酶活性的新机制,具有一定意义。
研究人员指出,NAD+依赖性蛋白去乙酰化酶SIRT1通过对包括组蛋白和转录因子在内的多种蛋白进行去乙酰化,在调节代谢,应激应答以及衰老方面发挥重要作用。调节SIRT1去乙酰化酶活性的机制非常复杂,但同时对于理解如何开发靶向SIRT1的治疗药物非常重要。
研究人员发现SIRT1的N端结构域(NTERM)能够通过与内源性SIRT1发生物理性相互作用对SIRT1的去乙酰化酶活性进行转激活,促进SIRT1与其去乙酰化酶底物NF-kB p65的结合。通过实验发现,SIRT1 N端结构域的两个基序对于激活SIRT1的酶活性具有重要作用,研究人员在小鼠中表达这些基序中的任一个都足以降低空腹血糖水平,提高葡萄糖耐受性,并且这种作用方式类似于SIRT1过表达的结果。
这些结果揭示了调节内源性SIRT1去乙酰化酶活性的一种新机制,同时对于如何通过药理学方法调节SIRT1活性提供了更加深入的见解。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#去乙酰化酶#
31
#CEL#
27
#结构域#
38
#Cell#
24
#sirt1#
36