近日,中国科学技术大学化学与材料科学学院梁高林教授课题组与中科院强磁场科学中心钟凯研究员课题组合作,发明一种能在化疗肿瘤内“智能”自聚集的磁共振纳米造影剂,并在患肿瘤的小鼠体内验证了其优异肿瘤成像效果。该研究成果3月31日在线发表在国际著名学术期刊《纳米快报》上。
半胱天冬酶家族在介导细胞凋亡的过程中起着重要的作用,对半胱天冬酶的检测可以很好地监测肿瘤细胞的早期凋亡,从而评价肿瘤化疗的疗效,为后续治疗提供参考。核磁共振成像是一种无放射、非侵入的影像学技术,且成像参数多、扫描速度快、组织分辨率高,是常见的影像检查方式。磁性纳米粒子在生物成像方面已经得到广泛应用,大的磁性纳米粒子比目前常用的小磁性氧化铁纳米粒子在磁共振成像方面更具优越性,但前者在血液中被很快清除,导致组织的磁共振信号降低。
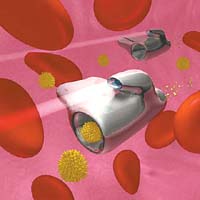
为解决这一难题,梁高林教授课题组设计了一种“智能”小分子——四氧化三铁复合纳米粒子,该纳米粒子在凋亡肿瘤细胞内半胱天冬酶的控制下,“智能”地自聚集成大尺寸磁性纳米粒子,可显著增强肿瘤的横向磁共振成像信号。他们与钟凯课题组合作,在中科院强磁场科学中心9.4特斯拉磁场强度下对小鼠肿瘤活体进行磁共振成像,结果显示,与对照组四氧化三铁磁性纳米粒子相比,该“智能”四氧化三铁磁性纳米粒子的横向加权磁共振成像信号显著增强,并且没有对小鼠产生毒性。
专家称,这种新型的四氧化三铁磁共振纳米造影剂,能够更加简单、准确和灵敏地测定体内外半胱天冬酶的活性,从而为肿瘤化疗疗效评价提供了新思路。审稿人高度评价了这一新颖的策略,称“这个新方法提供了一个很有价值的生物标志物用于肿瘤的成像和抗癌治疗疗效的检测”。
原始出处:
Yuan Y, Ding Z, Qian J, Zhang J, Xu J, Dong X, Han T, Ge S, Luo Y, Wang Y, Zhong K, Liang G. Casp3/7-Instructed Intracellular Aggregation of Fe3O4 Nanoparticles Enhances T2 MR Imaging of Tumor Apoptosis. Nano Lett. 2016 Apr 13;16(4):2686-91
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#曙光#
29
#评价#
33
#成像技术#
31
能生物治疗吗
121
文章不错
114
值得关注
107